Recommendations Published online in Annals of
the Rheumatic Diseases Propose That Physicians Consider Earlier
Intervention with Therapies Including LUPKYNIS® (voclosporin) as a
New LN Treatment Paradigm
Aurinia Pharmaceuticals Inc. (NASDAQ: AUPH) (Aurinia or the
Company) – Aurinia welcomes the 2023 updated recommendations from
The European Alliance of Associations for Rheumatology (EULAR) for
the management of systemic lupus erythematosus (SLE) based on
emerging new evidence, including a new treatment paradigm for lupus
nephritis (LN).
The new recommendations suggest that in addition to traditional
anchor drugs, therapies including LUPKYNIS® (voclosporin) should be
considered for any active class of lupus nephritis. Combination
therapy can be used first-line (i.e., in treatment-naïve patients).
If combination therapy is not used first-line, then add-on
treatment with therapies, including voclosporin, should be
considered if adequate response is not achieved within three to six
months or in patients who experience disease flare. In most cases,
patients should continue the therapy they were initially treated
with for at least three years following treatment response,
including voclosporin, as the guidelines cited the stable estimated
glomerular filtration rate (eGFR, an important measurement of
kidney function) observed with voclosporin over 3 years.
Importantly, the recommendations suggest that 5 mg/day should
serve as the highest acceptable maintenance dose of steroids in SLE
or LN (previous recommendations suggested achieving <=7.5 mg/day
by three to six months of LN treatment). This recommendation was
based on the significantly lower glucocorticoid doses used in
recent randomized clinical trials, including the AURORA clinical
studies of voclosporin.
The recommendations highlight the profound repercussions of
delaying diagnosis, thus recommending vigilant monitoring for new
organ damage, especially lupus nephritis, at every visit (at least
yearly).
“Aurinia appreciates EULAR’s thoughtful consideration for
improving the management of lupus nephritis with recommendations
that reflect therapeutic advancements in this underserved patient
population. The updated recommendations reflect the growing
recognition of the clinical value that a therapy like voclosporin
provides to people living with lupus nephritis. These
recommendations provide clear guidance for the importance of
initial therapy with voclosporin plus standard of care to preserve
kidney health in patients with active LN without reliance on
chronic high-dose glucocorticoids,” said Dr. Greg Keenan, Chief
Medical Officer of Aurinia.
For the 2023 updated recommendations, a task force of global SLE
experts, including 35 rheumatologists and five nephrologists, were
assembled to conduct a systematic literature review. The task force
agreed on five overarching principles and condensed recommendations
to a total of 13. The task force placed significant emphasis on a
shift in LN treatment strategies, advocating for the earlier and
more frequent use of immunosuppressants with the aim of reducing
patient reliance on steroids.
According to the recommendations, the pace of new developments
in SLE has accelerated over the last five years and the field of LN
has also witnessed advancements for the option of earlier use of
combination therapies, with the goal of reducing the reliance on
steroids. These advancements have encouraged the consideration of a
paradigm shift in the treatment of LN, moving from the traditional
induction-maintenance regimen to the early use of combination
therapies. These observations created the impetus for an update of
the recommendations, to provide guidance on an evolving landscape
and capitalize on the experience gained thus far.
The recommendations were based on the understanding that LN is a
severe disease by nature and is associated with worse rates of
mortality and morbidity. LN causes nephron loss over time that can
lead to chronic kidney disease and end-stage renal disease. Given
the consistently low rates of complete response at one to two years
of treatment observed in the control arms of LN clinical trials
(i.e., 20-30%), the option for additional therapy upfront should be
considered. Since recently approved therapies are indicated for all
adult patients with active LN, it was deemed reasonable that they
be considered as a first-line option.
The recommendations noted that the final decision for the
treatment of active LN should depend on the individual patient
characteristics, such as histological class, baseline eGFR,
proteinuria, presence of extrarenal manifestations, comorbidities,
risk for toxicity, access to drugs and cost issues, and patient
preferences.
About the AURORA Clinical Program In AURORA 1
(NCT03021499), a 12-month, phase 3, double-blind,
randomized-controlled pivotal study, the efficacy and safety of
voclosporin was compared with a control group in achieving complete
renal response (CRR) in patients with LN. AURORA 1 demonstrated the
clinical superiority of voclosporin with mycophenolate mofetil
(MMF) and low-dose glucocorticoids compared to MMF and low-dose
glucocorticoids alone. Significantly more patients in the
voclosporin group achieved a CRR at 52 weeks of treatment and did
so significantly faster than those in the control group. The safety
profile in AURORA 1 was comparable between treatment groups, in
line with previous studies; no new safety concerns were observed.
Results from the completed Phase 3 randomized, double-blind,
placebo-controlled, multicenter AURORA 1 study were published in
The Lancet.
AURORA 2 (NCT03597464) is a Phase 3, double-blind, extension
study to assess the long-term safety and tolerability of
voclosporin, in addition to MMF and low-dose glucocorticoids, for
the treatment of patients with active LN. Patients who completed 12
months of treatment in the Phase 3 AURORA 1 study were eligible to
enroll in the AURORA 2 extension study with the same randomized
treatment of voclosporin or placebo, in combination with MMF
(target dose of 2 g/day) and low-dose glucocorticoids (target dose
of ≤2.5 mg/day), for an additional 24 months.
A total of 216 LN patients continued into the extension study,
with 116 patients in the voclosporin group and 100 patients in the
control group; 90 and 78 patients, respectively, received 36 months
of total treatment at the completion of the study. Study drug dose
changes decreased over time.
Voclosporin was well tolerated with no new or worsening safety
signals in the extension study. Clinical efficacy over three years
of treatment was maintained, as observed by maintenance of urine
protein creatinine ratio (UPCR) reductions, sustained CRR and
preserved kidney function, suggesting a positive benefit-risk
profile for voclosporin in LN patients. These results were achieved
with most patients in both groups (>75%) maintaining
glucocorticoid tapering throughout the study and receiving doses of
≤2.5 mg/day at the end of the extension study.
AURORA 2 results were published in Arthritis & Rheumatology,
the official peer-reviewed journal of the American College of
Rheumatology.
About Lupus Nephritis Lupus Nephritis is a serious
manifestation of systemic lupus erythematosus (SLE), a chronic and
complex autoimmune disease. About 200,000-300,000 people live with
SLE in the U.S., and about one-third of these people are diagnosed
with lupus nephritis at the time of their SLE diagnosis. About 50
percent of all people with SLE may develop lupus nephritis. If
poorly controlled, lupus nephritis can lead to permanent and
irreversible tissue damage within the kidney. Black and Asian
people with SLE are four times more likely to develop lupus
nephritis and Hispanic people are approximately twice as likely to
develop the disease, compared to White people with SLE. Black and
Hispanic people with SLE also tend to develop lupus nephritis
earlier and have worse outcomes, compared to White people with
SLE.
About LUPKYNIS® LUPKYNIS® is the first U.S. Food and Drug
Administration and European Commission-approved oral medicine for
the treatment of adult patients with active LN. LUPKYNIS is a
novel, structurally modified calcineurin inhibitor (CNI) with a
dual mechanism of action, acting as an immunosuppressant through
inhibition of T-cell activation and cytokine production and
promoting podocyte stability in the kidney. The recommended
starting dose of LUPKYNIS is three capsules twice daily with no
requirement for serum drug monitoring. Dose modifications can be
made based on Aurinia’s proprietary personalized eGFR-based dosing
protocol. Boxed Warning, warnings, and precautions for LUPKYNIS are
consistent with those of other CNI-immunosuppressive
treatments.
About Aurinia Aurinia Pharmaceuticals is a fully
integrated biopharmaceutical company focused on delivering
therapies to treat targeted patient populations with high unmet
medical needs that are impacted by autoimmune, kidney and rare
diseases. In January 2021, the Company introduced LUPKYNIS®
(voclosporin), the first FDA-approved oral therapy dedicated to the
treatment of adult patients with active lupus nephritis. The
Company’s head office is in Edmonton, Alberta, its U.S. commercial
office is in Rockville, Maryland. The Company focuses its
development efforts globally.
INDICATION AND IMPORTANT SAFETY INFORMATION
INDICATIONS LUPKYNIS® is indicated in combination with a
background immunosuppressive therapy regimen for the treatment of
adult patients with active LN. Limitations of Use: Safety and
efficacy of LUPKYNIS have not been established in combination with
cyclophosphamide. Use of LUPKYNIS is not recommended in this
situation.
IMPORTANT SAFETY INFORMATION
BOXED WARNINGS: MALIGNANCIES AND SERIOUS INFECTIONS
Increased risk for developing malignancies and serious infections
with LUPKYNIS or other immunosuppressants that may lead to
hospitalization or death.
CONTRAINDICATIONS LUPKYNIS is contraindicated in patients
taking strong CYP3A4 inhibitors because of the increased risk of
acute and/or chronic nephrotoxicity, and in patients who have had a
serious/severe hypersensitivity reaction to LUPKYNIS or its
excipients.
WARNINGS AND PRECAUTIONS Lymphoma and Other Malignancies:
Immunosuppressants, including LUPKYNIS, increase the risk of
developing lymphomas and other malignancies, particularly of the
skin. The risk appears to be related to increasing doses and
duration of immunosuppression rather than to the use of any
specific agent. Serious Infections: Immunosuppressants, including
LUPKYNIS, increase the risk of developing bacterial, viral, fungal,
and protozoal infections (including opportunistic infections),
which may lead to serious, including fatal, outcomes.
Nephrotoxicity: LUPKYNIS, like other CNIs, may cause acute
and/or chronic nephrotoxicity. The risk is increased when CNIs are
concomitantly administered with drugs associated with
nephrotoxicity. Hypertension: Hypertension is a common adverse
reaction of LUPKYNIS therapy and may require antihypertensive
therapy.
Neurotoxicity: LUPKYNIS, like other CNIs, may cause a spectrum
of neurotoxicities: severe include posterior reversible
encephalopathy syndrome (PRES), delirium, seizure, and coma; others
include tremor, paresthesia, headache, and changes in mental status
and/or motor and sensory functions.
Hyperkalemia: Hyperkalemia, which may be serious and require
treatment, has been reported with CNIs, including LUPKYNIS.
Concomitant use of agents associated with hyperkalemia may increase
the risk for hyperkalemia.
QTc Prolongation: LUPKYNIS prolongs the QTc interval in a
dose-dependent manner when dosed higher than the recommended lupus
nephritis therapeutic dose. The use of LUPKYNIS in combination with
other drugs that are known to prolong QTc may result in clinically
significant QT prolongation. Immunizations: Avoid the use of live
attenuated vaccines during treatment with LUPKYNIS. Inactivated
vaccines noted to be safe for administration may not be
sufficiently immunogenic during treatment with LUPKYNIS.
Pure Red Cell Aplasia: Cases of pure red cell aplasia (PRCA)
have been reported in patients treated with another CNI
immunosuppressant. If PRCA is diagnosed, consider discontinuation
of LUPKYNIS. Drug-Drug Interactions: Avoid co-administration of
LUPKYNIS and strong CYP3A4 inhibitors or with strong or moderate
CYP3A4 inducers. Reduce LUPKYNIS dosage when co-administered with
moderate CYP3A4 inhibitors. Reduce dosage of certain P-gp
substrates with narrow therapeutic windows when
co-administered.
ADVERSE REACTIONS The most common adverse reactions
(>3%) were glomerular filtration rate decreased, hypertension,
diarrhea, headache, anemia, cough, urinary tract infection,
abdominal pain upper, dyspepsia, alopecia, renal impairment,
abdominal pain, mouth ulceration, fatigue, tremor, acute kidney
injury, and decreased appetite.
SPECIFIC POPULATIONS Pregnancy/Lactation: May cause fetal
harm. Advise not to breastfeed. Renal Impairment: Not recommended
in patients with baseline eGFR ≤45 mL/min/1.73 m2 unless benefit
exceeds risk. Severe renal impairment: Reduce LUPKYNIS dose.
Mild and Moderate Hepatic Impairment: Reduce LUPKYNIS dose.
Severe hepatic impairment: Avoid LUPKYNIS use.
Please see Prescribing Information, including Boxed Warning, and
Medication Guide for LUPKYNIS.
References Fanouriakis A, Kostopoulou M, Andersen J, et
al. EULAR recommendations for the management of systemic lupus
erythematosus: 2023 update. Annals of the Rheumatic Diseases.
Published Online First: 12 October 2023. doi:
10.1136/ard-2023-224762.
View source
version on businesswire.com: https://www.businesswire.com/news/home/20231026228518/en/
Media Inquiries: Andrea Christopher, Corporate
Communications Director, Aurinia achristopher@auriniapharma.com
Investor Inquiries: ir@auriniapharma.com
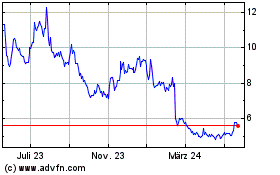
Aurinia Pharmaceuticals (NASDAQ:AUPH)
Historical Stock Chart
Von Nov 2024 bis Dez 2024
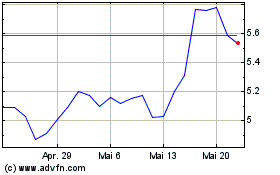
Aurinia Pharmaceuticals (NASDAQ:AUPH)
Historical Stock Chart
Von Dez 2023 bis Dez 2024