false
0001679049
true
0001679049
2024-12-26
2024-12-26
0001679049
us-gaap:CommonStockMember
2024-12-26
2024-12-26
0001679049
insw:RightscommonstockMember
2024-12-26
2024-12-26
iso4217:USD
xbrli:shares
iso4217:USD
xbrli:shares
UNITED
STATES
SECURITIES
AND EXCHANGE COMMISSION
Washington,
D.C. 20549
FORM
8-K
CURRENT
REPORT
PURSUANT
TO SECTION 13 OR 15(d) OF THE
SECURITIES
EXCHANGE ACT OF 1934
December 31, 2024 (December 26, 2024)
Date of Report (Date
of earliest event reported)
International Seaways, Inc.
(Exact Name of Registrant
as Specified in Charter)
1-37836-1
Commission File Number
| Marshall Islands |
|
98-0467117 |
(State or other jurisdiction of
incorporation or organization) |
|
(I.R.S. Employer Identification Number) |
600 Third Avenue,
39th Floor
New York, New York
10016
(Address
of Principal Executive Offices) (Zip Code)
(212)
578-1600
Registrant's telephone
number, including area code
Check the appropriate box below if the Form 8-K filing is intended to simultaneously satisfy the filing obligation of the registrant under any of the following provisions:
| ¨ | Written communications pursuant to Rule 425 under the
Securities Act (17 CFR 230.425) |
| ¨ | Soliciting material pursuant to Rule 14a-12 under the
Exchange Act (17 CFR 240.14a-12) |
| ¨ | Pre-commencement communications pursuant to Rule 14d-2(b)
under the Exchange Act (17 CFR 240.14d-2(b)) |
| ¨ | Pre-commencement communications pursuant to Rule 13e-4(c)
under the Exchange Act (17 CFR 240.13e-4(c)) |
Indicate by check mark whether the registrant is an emerging growth company as defined in Rule 405 of the Securities Act of 1933 (§230.405 of this chapter) or Rule 12b-2 of the Securities Exchange Act of 1934 (§240.12b-2 of this chapter).
Emerging
growth company ¨
If
an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for
complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ¨
Securities registered pursuant to Section 12(b)
of the Act:
| Title of each class |
Symbol |
Name of each exchange on which registered |
| Common Stock (no par value) |
INSW |
New York Stock Exchange |
| Rights to Purchase Common Stock |
N/A true |
New York Stock Exchange |
| Item 5.02(e) | Departure of Directors or Certain Officers; Election of Directors;
Appointment of Certain Officers; Compensatory Arrangements of Certain Officers. |
The Board of Directors (the “Board”)
of International Seaways, Inc. (the “Company”) has determined that it was in the best interests of the Company
to terminate the International Seaways, Inc. Retiree Health and Welfare Plan (the “Plan”) and distribute all amounts
deferred under the Plan to participants.
On December 26, 2024, the Board elected to
terminate the Plan pursuant to its terms, as set forth in the First Amendment to the Plan. All accrued and unpaid benefits in the Plan
are expected to be distributed in compliance with the plan distribution requirements set forth in Treasury Regulation 1.409A 3(j)(4)(ix)(C) under
the general plan termination rule of Section 409A. Such benefits are expected to be paid no earlier than 12 months, and
no later than 24 months, following the termination date.
The foregoing description of the amendment to
the Plan is qualified in its entirety by reference to the full text of the amendment set forth in Exhibit 10.1 to this Current Report
on Form 8-K and incorporated herein by reference.
| Item 9.01 | Financial Statements and
Exhibits |
SIGNATURES
Pursuant to the requirements of the Securities
Exchange Act of 1934, the Registrant has duly caused this report to be signed on its behalf by the undersigned hereunto duly authorized.
| |
INTERNATIONAL SEAWAYS, INC. |
| |
(Registrant) |
| |
|
| Date: December 31, 2024 |
By: |
|
/s/ James D. Small III |
| |
|
Name: |
James D. Small III |
| Title: |
Chief Administrative Officer, Senior Vice President, Secretary and General Counsel |
EXHIBIT INDEX
Exhibit 10.1
First Amendment to OSG Ship Management, Inc.
Retiree Health and Welfare Plan
This First Amendment (the
“Amendment”) hereby amends, effective as of December 31, 2024, the International Seaways, Inc. Retiree Health and
Welfare Plan (the “Plan”) to include the following provision under Article 6. Capitalized terms used herein and not defined
herein have the meanings set forth in the Plan.
6.3 Plan
Termination and Liquidation. Notwithstanding anything to the contrary in the Plan, the Plan shall terminate as of December 31,
2024 (the “Termination Effective Date”), and no further amounts shall be deferred under the Plan after such date. Each Participant’s
accrued and unpaid benefits (determined on a present value basis through age 65) shall be paid to such Participant in a single lump sum
payment as soon as administratively practicable following the one-year anniversary of the Termination Effective Date, but in no case later
than twenty-four (24) months after the Termination Effective Date, provided that benefits payable under the Plan prior to the liquidation
date if no action had been taken to terminate the Plan shall be paid in accordance with their original schedule. This paragraph shall
be construed and interpreted in a manner to comply with the requirements of Treasury Regulation section 1.409A-3(j)(4)(ix)(C).
Exhibit 99.1
Amended and Restated as of December 26,
2024
INTERNATIONAL SEAWAYS RETIREE HEALTH AND WELFARE
PLAN
and
SUMMARY PLAN DESCRIPTION
Effective as of January 1, 2017
TABLE OF CONTENTS
Page
| ARTICLE 1 |
ELIGIBILITY |
|
| 1.1 |
Eligibility for Coverage |
6 |
| 1.2 |
Service |
6 |
| 1.3 |
Medical and Health Benefits |
6 |
| 1.4 |
Death Benefit |
7 |
| |
|
|
| ARTICLE 2 |
PARTICIPATION &
COVERAGE FOR MEDICAL AND HEALTH BENEFITS |
|
| |
|
|
| 2.1 |
Enrollment |
7 |
| 2.2 |
Benefits |
7 |
| 2.3 |
Eligible Medical Expenses |
8 |
| 2.4 |
Medicare Coverage |
9 |
| 2.5 |
Dependent Coverage |
10 |
| 2.6 |
Termination of Benefits |
10 |
| 2.7 |
Receiving Reimbursements from Your HRA account |
10 |
| 2.8 |
Overpayments |
10 |
| 2.9 |
In the Event of Your Death |
11 |
| |
|
|
| ARTICLE 3 |
COBRA |
|
| |
|
|
| 3.1 |
COBRA Coverage |
11 |
| |
|
|
| ARTICLE 4 |
PAYMENT OF BENEFITS |
|
| |
|
|
| 4.1 |
Payments for Incompetent Persons |
13 |
| 4.2 |
Qualified Medical Child Support Orders |
13 |
| |
|
|
| ARTICLE 5 |
ADMINISTRATION OF THE PLAN |
|
| |
|
|
| 5.1 |
Named Fiduciary |
13 |
| 5.2 |
Allocation of Responsibilities |
14 |
| 5.3 |
Liability for Allocated Responsibilities |
14 |
| 5.4 |
Actions of the Company to be Uniform; Regular Personnel
Policies to be Followed |
15 |
| 5.5 |
Committee |
15 |
| 5.6 |
Decisions of Committee are Binding |
15 |
| 5.7 |
Delegation of Authority |
15 |
| 5.8 |
Reliance on Various Documents |
15 |
| 5.9 |
Accounts and Records |
16 |
| 5.10 |
Compliance with Applicable Law |
16 |
| 5.11 |
Liability |
16 |
| 5.12 |
Indemnification |
16 |
| 5.13 |
Claims Procedure |
17 |
| 5.14 |
Initial Claims and Review Procedures |
17 |
| 5.15 |
Benefits |
20 |
| 5.16 |
Limitations Period |
21 |
| 5.17 |
Venue |
21 |
| 5.18 |
Electronic Administration |
21 |
| |
|
|
| ARTICLE 6 |
AMENDMENT AND TERMINATION |
|
| |
|
|
| 6.1 |
Amendment and Termination |
21 |
| 6.2 |
Effect of Amendment or Termination |
21 |
| 6.3 |
Plan Termination and Liquidation |
22 |
| |
|
|
| ARTICLE 7 |
MISCELLANEOUS |
|
| |
|
|
| 7.1 |
Funded Status of Plan |
22 |
| 7.2 |
Prohibition of Discrimination |
22 |
| 7.3 |
Exclusive Benefit |
22 |
| 7.4 |
Restriction Against Assignment |
22 |
| 7.5 |
No Vested Interest |
23 |
| 7.6 |
Action to Comply with Law |
23 |
| 7.7 |
Subrogation |
23 |
| 7.8 |
Coverage and Military Duty in the U.S. Armed Forces |
24 |
| 7.9 |
Women’s Health and Cancer Rights Act |
24 |
| 7.10 |
Newborns’ and Mothers’ Health Protection Act |
25 |
| 7.11 |
Titles and Headings |
25 |
| 7.12 |
Applicable Law |
25 |
| 7.13 |
Conflicts |
25 |
| 7.14 |
PBGC |
25 |
| |
|
|
| ARTICLE 8 |
HIPAA INFORMATION |
|
| |
|
|
| 8.1 |
HIPAA Privacy Provisions |
25 |
| 8.2 |
HIPAA Security Provisions |
27 |
| 8.3 |
Mitigation |
28 |
| 8.4 |
Breach Notification |
28 |
| |
|
|
| ARTICLE 9 |
YOUR RIGHTS UNDER ERISA AND OTHER LAWS |
29 |
| |
|
|
| ARTICLE 10 |
ADDITIONAL INFORMATION |
31 |
| |
|
|
| APPENDIX |
HEALTH REIMBURSEMENT ACCOUNTS |
A-1 |
PREFACE
International Seaways Ship Management LLC (the
“Company”) maintains the International Seaways Retiree Health and Welfare Plan (the “Plan”) to
provide designated health and welfare benefits to eligible retirees of the Company or of International Seaways, Inc.
(“Parent”, and each of Parent and the Company, an “Employer”) and their Eligible Dependents
(as defined in Article 2). For the avoidance of doubt, Parent is an affiliate of the Company for all purposes hereunder.
Benefits under the Plan are available only to retirees
meeting the requirements described in Article 1 and their Eligible Dependents. This document and/or other documentation describing
the health and welfare programs available to eligible retirees and their Eligible Dependents are intended to constitute one single Plan
document and summary plan description (“SPD”) for purposes of the reporting and disclosure requirements of the Employee
Retirement Income Security Act of 1974, as amended (“ERISA”) and the Internal Revenue Code of 1986, as amended (the
“Code”).
The Company is the Plan Administrator. The Company
has designated and appointed a person or person(s), referred to herein as the Committee, to administer the Plan on its behalf. As of June 30,
2018, and until such time as the Company may designate new or additional members of the Committee, the Committee is comprised of Messrs. Steven
Stulbaum, James Small and Scott Godec.
This Plan covers only retired employees (also referred
to as “retirees”) of an Employer who otherwise meet all the eligibility and participation requirements under the Plan, but
in some instances also will apply to an Eligible Dependent of such a retiree. Notwithstanding any provision of the Plan to the contrary,
in no event will a current employee of the Company or any of its affiliates be eligible to be a participant in the Plan. If a participant
in the Plan becomes a current employee of the Company or any of its affiliates, such person will immediately become ineligible for the
Plan and will cease participation in the Plan in all respects, unless and until such person subsequently retires again, at which time
their eligibility to participate in the Plan at that time shall be determined in accordance with the terms of the Plan. For the avoidance
of doubt, any person who was not a retiree prior to the spin-off of the Parent from OSG (as defined below) on November 30, 2016 (the
“Spin-Off”) and who was employed by an Employer after the Spin-Off did not become a retiree solely by virtue of the
Spin-Off.
Among other matters, this Plan provides
benefits to certain retirees from the Employers which accrued through November 30, 2016 under the OSG Ship
Management, Inc. Retiree Health and Welfare Plan dated January 1, 2012 as amended from time to time (as so amended, the
“OSG Retiree Health Plan”). In connection with the Spin-off, and that certain Employee Matters Agreement by and
among OSG and the Parent dated as of November 30, 2016, the Parent has assumed certain obligations under the OSG Retiree Health
Plan with respect to certain persons eligible for benefits thereunder (the “Transferred Retirees”). Generally,
Transferred Retirees were employed in connection with the International Flag business of OSG for periods prior to the Spin-Off,
subject to the requirements specified in Section 1.1 (Eligibility for Coverage) below and the other terms and conditions of the
Plan and the OSG Retiree Health Plan.
The Plan is intended to
constitute a plan covering “less than two participants who are current employees” for purposes of the Patient Protection
and Affordable Care Act, as amended by the Health Care and Education Reconciliation Act of 2010 (collectively, the
“Affordable Care Act”). As such, most provisions of the Affordable Care Act do not apply to the Plan.
Notwithstanding the foregoing, to the extent any requirements of the Affordable Care Act still impact the Plan, the Plan is to be
administered and interpreted in a manner consistent therewith.
The term “you” as used in this
Plan document and SPD generally refers to a retiree of an Employer who otherwise meets all the eligibility and participation requirements
under the Plan, but in some instances also will apply to an Eligible Dependent of such a retiree. Receipt of this Plan document and SPD
does not guarantee that the recipient is in fact a participant under the Plan and/or is otherwise eligible for benefits under the Plan.
The following document sets forth the terms and
provisions of the Plan in effect as of January 1, 2017.
ARTICLE 1
ELIGIBILITY
| 1.1 | Eligibility for Coverage. You are eligible for coverage under the Plan if: |
| (A) | you were hired by Overseas Shipholding Group, Inc. or one of its affiliates (collectively, “OSG”)
prior to January 1, 2005, as an active employee; and |
| (B) | you were enrolled on your date of retirement in the medical plan: (1) for active employees sponsored
by the Company, (2) in which the Company or any of its affiliates or co-employers participate, or (3) for active employees sponsored
by OSG; and |
| (C) | (i) as of December 1, 2016, you were retired and had met the Plan’s age and service requirements specified below based
on your date of retirement, and retired from OSG while working in the lines of business that became an Employer following the Spin-Off;
or |
(ii) you
were part of the group of employees that as of November 30, 2016, were spun-off to an Employer by OSG in the Spin-Off and you meet
the Plan’s age and service requirements specified below at the time of your retirement.
| · | Age and Service Requirements. To be eligible for benefits under this Plan, you must be at least 55 years of age with at least
10 years of Credited Service as of your retirement date. Further you must have retired from an Employer or have retired from OSG while
working in the lines of business that became an Employer following the Spin-Off. |
Maritrans.
Please note that employees originally employed by Maritrans, Inc. who became employees of OSG following the acquisition of Maritrans, Inc.
by OSG are not eligible for coverage under this Plan.
| 1.2 | Service. For purposes of determining your eligibility for coverage under the Plan, |
| · | “Actual Service” means your period of actual service with an Employer or OSG beginning with your employment
date, without any intervening breaks in your service or leave of absences. However, periods of employment with such an employer with a
break in service that is 365 days or less will still be considered to be continuous. If, however, your break in service exceeds 365 days,
your prior service will not count toward your Actual Service for purposes of eligibility for, or amount of, coverage under the Plan. |
| · | “Credited Service” means your period of Actual Service, provided that Credited Service means two times your
Actual Service with OSG or one of its affiliates prior to January 1, 1991, plus your Actual Service with OSG or an Employer after
December 31, 1990. |
1.3 Medical
and Health Benefits. If you are an Eligible Retiree covered under the Plan, you and your Eligible Dependents (as described in
Article 2) will be eligible for reimbursement of your payment of certain medical and health expenses. More information is
provided in Article 2 and the Appendix.
1.4 Death
Benefit. If you are an Eligible Retiree covered under the Plan, the Company will provide $10,000 of death benefits on your life. This
benefit is expected to be paid in the year following the year of your death. Death benefits are not paid on behalf of your Eligible Dependents.
ARTICLE 2
PARTICIPATION & COVERAGE FOR MEDICAL
AND HEALTH BENEFITS
2.1 Enrollment.
If you satisfy the requirements set forth in Section 1.1, you will be eligible for retiree health coverage when you retire. You will
have the following options:
| · | Enroll in the Plan, and Coverage Will Begin at Retirement: Benefits start on the first day of the
month after the date of retirement, for yourself and your Eligible Dependents (if applicable). Your coverage remains in effect until your
coverage under the Plan ends or you suspend or drop your coverage, as described below. |
| · | Waive Coverage Under the Plan: You may decline coverage under the Plan at retirement or may drop coverage under the Plan at
any time after retirement. If you decline or drop coverage, you will be considered to have permanently waived your right to retiree health
care benefits, and you will not be permitted to elect coverage under the Plan in the future. |
However, if you have medical coverage as an employee
of another employer, you may elect to suspend coverage under the Plan for you and your Eligible Dependents. To suspend coverage, you must
furnish written proof of other medical coverage for you within 31 days of the suspension of coverage. To be reinstated, you must make
written application for a reinstatement within 31 days of the termination of other medical coverage and furnish written proof of when
the other medical coverage terminated. The reinstatement will be effective on the day following the termination of other medical coverage.
(a) Health
benefits coverage under this Plan will be provided through a Health Reimbursement Arrangement account (“HRA”), as more
fully described in the Appendix. The HRA will reimburse you for Eligible Medical Expenses for you and your Eligible Dependents, up
to the amount available in your HRA account. Reimbursements for Eligible Medical Expenses paid by your HRA account generally are
intended to be excludable from your taxable income. However, neither the Company nor any of its employees or affiliates can
guarantee the tax treatment to any given HRA Participant (as defined in the Appendix), as individual circumstances may produce
different results. If there is any doubt, you should consult your own tax advisor.
(b) Your
HRA account is a bookkeeping account on the Company’s records; it is not funded and does not bear interest or accrue earnings
of any kind. All benefits are paid entirely from the Company’s general assets. Your HRA account will be credited with Company
contributions as described in the Appendix, and then will be debited for each reimbursement to you or your Eligible Dependent of
Eligible Medical Expenses approved by the Company’s Human Resources department or its delegate. Each Plan Year that you are
eligible to participate in the HRA, your HRA will be credited with the amount described in the Appendix. If you do not use all of
the amount credited to your HRA account during a Plan Year, the unused portion will be carried over for reimbursement of Eligible
Medical Expenses incurred in subsequent Plan Years (as long as you continue to participate in the Plan). Any unused funds in your
HRA when neither you or your Eligible Dependents are eligible for further reimbursements from the HRA will be forfeited by the HRA
and returned to the Company.
(c) The
annual amount that will be contributed to the HRA account of an Eligible Retiree is specified in the Appendix, as it may be amended
from time to time. Employer contributions may be made on an annual, quarterly, monthly or other basis as the Company determines in
its sole discretion. When a retiree first becomes eligible for this Plan, the Human Resources Department will notify him or her
regarding the then-current timing of Employer contributions, and also will notify him or her if the timing subsequently is modified.
For the year in which the Eligible Retiree attains age 65, the annual Employer contribution will be pro-rated for the portions of
the year before and after entry into the Plan or age 65, as the case may be. Employer contributions will cease upon the death of the
Eligible Retiree.
| 2.3 | Eligible Medical Expenses. |
An “Eligible Medical Expense”
generally is an expense incurred by an Eligible Retiree or an Eligible Dependent for medical care, as that term is defined in Code Section 213(d) (generally,
they are expenses related to the diagnosis, care, mitigation, treatment or prevention of disease). Such expenses typically include physician,
hospital, dental, vision or pharmacy expenses. Only Eligible Medical Expenses incurred by Eligible Retirees or Eligible Dependents may
be reimbursed from an HRA account. Eligible Medical Expenses are “incurred” when the medical care is provided, not when you
are billed, charged or pay for the expense. Thus, an expense that has been paid but not incurred (e.g. pre-payment to a physician) will
not be reimbursed until the services or treatment giving rise to the expense has been provided. Some common examples of Eligible Medical
Expenses include:
| · | Medications prescribed by a doctor (even if the medication is available without a prescription) or insulin; |
| · | Contact lenses or glasses used to correct a vision impairment; |
| · | Chiropractor treatments; |
| · | Premiums for medical (e.g., Medicare Part B, Medicare Supplement or COBRA), prescription drug, dental, vision or long-term care
insurance that have not been purchased with pre-tax dollars. |
Some examples of common items that are not Eligible Medical
Expenses include:
| · | Expenses incurred prior to the date that you became a participant in the Plan; |
| · | Expenses incurred after the date that you cease to be a participant in the Plan (unless COBRA coverage is timely and properly elected),
other than Eligible Medical Expenses incurred not later than December 31 of the year following the year of your death by your surviving
Eligible Dependent while he or she is covered by the Plan after your death and for which sufficient funds remain in your HRA account; |
| · | Annual medical contract fees for exclusive provider care; |
| · | Babysitting and child care; |
| · | Cosmetic surgery or similar procedures (unless the surgery is necessary to correct a deformity arising from a congenital abnormality,
accident or disfiguring disease); |
| · | Funeral and burial expenses; |
| · | Household and domestic help; |
| · | Health club or fitness program dues; |
| · | Cosmetics, toiletries, toothpaste, etc.; |
| · | Expenses paid with pre-tax dollars; and |
| · | Expenses that have been reimbursed (or paid directly) by another plan or for which you (or, if applicable, your Eligible Dependents)
are eligible to seek reimbursement (or direct payment) under another health plan. |
For more information about what items are and are not
Eligible Medical Expenses, consult IRS Publication 502, “Medical and Dental Expenses,” under the headings “What
Medical Expenses Are Includible” and “What Expenses Aren’t Includible.” Be careful in relying on this IRS
Publication, however, as it is specifically designed to address what medical expenses are deductible on Form 1040, Schedule A,
but not what is reimbursable under a health reimbursement account. If you need more information regarding whether an expense is an
eligible medical expense under the Plan, contact the Company’s Human Resources Department.
2.4 Medicare
Coverage. Medicare coverage should be applied for in a timely manner by contacting the Social Security Administration at least 90
days before the date you are eligible to receive Medicare benefits. If you remain an active employee after age 65, there will be no penalty
for late enrollment in Medicare (Part B). However, it is important that you enroll in Medicare (Part B) in advance of your retirement
after age 65 since Medicare is considered your primary health insurance carrier upon termination of employment or on the first of the
month following your termination of employment. In any case, you should consider applying for Medicare (Part A – Hospital)
coverage prior to reaching age 65. Also remember that the Company contributions to your HRA account are reduced after you attain age 65,
as if you had become enrolled in Medicare at that time.
2.5 Dependent
Coverage. You may use your HRA account for Eligible Medical Expenses of your Eligible Dependents, i.e., your spouse and your dependent
children as described below.
| (a) | Your “spouse” is the person you are married to, and not legally separated from, on the date the expense
is incurred. |
| (b) | Your “dependent children” are your unmarried children who are related to you by blood, adoption or marriage,
and for whom you have assumed a legal obligation and who normally reside in your household in a parent-child relationship. In addition,
the children must be dependent upon you for support and maintenance, regardless of their status on the last day of your employment with
the Company. Children must be under 27 years of age as of December 31 of the year in question except for unmarried children who are
dependent on you for support and are permanently and totally disabled (as defined in Code Section 22(e)(3); proof of such status
may be required). |
Eligible
Dependent: “Eligible Dependent,” as used throughout this Plan and SPD, means your spouse or dependent
child who meets the conditions described in (a) or (b) above.
2.6 Termination
of Benefits. Your benefits under the Plan will continue for the duration of your life, subject to the terms of the Plan, including
the amendment and termination provisions under Section 6.1 of the Plan. Subject to COBRA rights, coverage of your Eligible Dependents
(i.e., ability to receive reimbursements from the HRA account, but not to receive additional Company contributions) will end as of December 31
of the year following the year of your death, to the extent sufficient funds remain in your HRA account after your death.
2.7 Receiving Reimbursements from Your
HRA account. You must complete a reimbursement form and mail or fax it to the Company’s Human Resources Department, along
with a copy of your insurance premium bill or “explanation of benefits” (“EOB”) or, if no EOB is
provided, a written statement from the service provider. The written statement from the service provider must contain the following:
(a) the name of the patient, (b) the date service or treatment was provided, (c) a description of the service or
treatment; and (d) the amount incurred.
Blank claim reimbursement forms are available from
the Company’s Human Resources Department. After your claim reimbursement form is completed, the form and supporting documentation
must be filed with the Company’s Human Resources Department within the time period described in the Appendix.
Your claim is deemed filed when it is
received by the Company’s Human Resources Department. If your claim for reimbursement is approved, you will be provided
reimbursement as soon as reasonably possible following the determination. Claims generally are paid in the order in which they are
received by the Company’s Human Resources Department.
2.8 Overpayments.
If it is later determined that you or your Eligible Dependent received an overpayment or a payment was made in error (e.g., you
were reimbursed from your HRA account for an expense that is later paid by another medical plan), you or your Eligible Dependents will
be required to refund the overpayment or erroneous reimbursement to the Employers.
If you do not refund the overpayment or erroneous
payment, the Employers reserve the right to offset future reimbursements equal to the overpayment or erroneous payment or, if that is
not feasible, to withhold such funds from any amounts due to you from the Employers. If all other attempts to recoup the overpayment or
erroneous payment are unsuccessful, the Plan Administrator may treat the overpayment or erroneous payment as a bad debt, which may have
tax implications for you.
2.9 In
the Event of Your Death. No further Company contributions will be made to your HRA account with respect to any period after your death.
If you die without an Eligible Dependent, any remaining
balance in your HRA account will be forfeited. However, your estate or representatives may submit claims for Eligible Medical Expenses
incurred by you before your death.
If you die with an Eligible Dependent, your HRA
account will not receive future Company contributions, but your Eligible Dependents can continue to submit for reimbursement their
claims for Eligible Medical Expenses incurred through December 31 of the year following the year of your death.
If your Eligible Dependent
later dies, his or her estate or representatives may submit claims for Eligible Medical Expenses incurred by your Eligible Dependent before
his or her death, but not later than December 31 of the year following the year of your death.
Claims for reimbursement must
be submitted within the time period specified in the Appendix.
ARTICLE 3
COBRA
3.1 COBRA
Coverage. If you or your Eligible Dependent are eligible to receive reimbursements from your HRA account and lose that coverage due
to a COBRA qualifying event, you or they will be entitled to continue the retiree coverage on a self-pay basis in accordance with COBRA
for a period of up to 18 months (for you) or up to 36 months (for them) from the date of the loss of retiree coverage.
A COBRA qualifying event for you would be a termination
of coverage due to the bankruptcy of the Company. A COBRA qualifying event for your Eligible Dependent would be a termination of coverage
due to your death, divorce (or legal separation) or the child’s no longer being considered a dependent child under the Plan.
You and your Eligible Dependents will have 60 days
from the later of: (i) the date of the loss of coverage because of the COBRA qualifying event, or (ii) the date you, he or she
is furnished with a COBRA Election Notice, to elect COBRA continuation coverage. Election Forms must be postmarked within that 60-day
period and must be received by the Plan Administrator. If COBRA continuation coverage is timely elected, coverage will begin on the date
that coverage under the Plan would otherwise have been lost due to the qualifying event.
If COBRA continuation coverage is timely elected
(and paid for), coverage will be provided that is substantially identical to the coverage being provided under the Plan prior to the qualifying
event. If COBRA continuation coverage is not timely elected (and paid for), health coverage under the Plan will end for the affected individual(s).
If coverage continues under COBRA, the cost will
be up to 102% of the Plan’s cost of coverage. The Plan Administrator will notify you and/or your Eligible Dependent (as the case
may be) of the cost of the coverage at the time you, he or she receives notice of entitlement to COBRA coverage, and will also provide
notice of any changes in the monthly COBRA premium amount. There will be a grace period of 45 days to pay the first premium payment, which
must include the premiums due for all months starting with the date retiree coverage ended and continuing through the date of payment.
If this payment is not made within 45 days of the date of the COBRA election, entitlement to COBRA continuation coverage will terminate.
After the initial premium payment, monthly premium payments are due on the first day of each month, and there will be a grace period of
30 days each month to make these payments. If a monthly payment is not made by the end of the applicable grace period, COBRA coverage
will terminate retroactive to the last date for which a timely payment for coverage was made. Premium payments must be postmarked within
the applicable grace period and must be received by the Plan Administrator or its delegate.
The law provides that COBRA continuation coverage
may be cut short prior to the expiration of the 36-month period for any of the following reasons:
1. The
group health coverage is terminated (and the Company is not required by COBRA to provide other group health coverage that it maintains,
if any);
2. The
premium for continuation coverage is not timely paid (within the applicable grace period);
3. The
individual first becomes, after electing COBRA coverage, covered under another group health plan (as an employee or otherwise) that does
not contain any preexisting condition exclusion or limitation applicable to the individual; or
4. The
individual becomes entitled to Medicare after electing COBRA coverage.
Continuation coverage may also be terminated for any reason the Plan
would terminate coverage of a participant or beneficiary not receiving continuation coverage (such as fraud).
Questions concerning the Plan or COBRA continuation
coverage rights should be addressed to the Company’s
Human Resources Department. For more information about your rights under ERISA, including COBRA, the Health Insurance Portability and
Accountability Act (HIPAA), and other laws affecting group health plans, contact the nearest Regional or District Office of the U.S.
Department of Labor’s Employee Benefits Security Administration (EBSA) in your area or visit the EBSA website at www.dol.gov/ebsa.
(Addresses and phone numbers of Regional and District EBSA Offices are available through EBSA’s website.)
In order to protect your Eligible
Dependents’ rights, you should keep the Company’s Human Resources Department informed of any changes in your address or
the addresses of family members. You should also keep a copy, for your records, of any notices you send to the Plan Administrator or
the Human Resources Department.
ARTICLE 4
PAYMENT OF BENEFITS
4.1 Payments
for Incompetent Persons. If the Committee determines that a benefit is payable to you, but that you are unable to care for your affairs
because of illness or accident, any payment due (unless a prior claim therefor will have been made by a duly appointed guardian, committee
or other legal representative) may be paid to your Spouse, child, grandchild, parent, brother or sister, or to any person deemed by the
Committee to have incurred expense for such person otherwise entitled to payment. If the Committee determines that a benefit is payable
to your Eligible Dependent, but that your Eligible Dependent is unable to care for his or her affairs because of illness or accident,
any payment due (unless a prior claim therefor will have been made by a duly appointed guardian, committee or other legal representative)
may be paid to you, your Spouse, child, grandchild, parent, brother or sister, or to any person deemed by the Committee to have incurred
expense for such person otherwise entitled to payment. Any such payment will be a complete discharge of any liability under the Plan therefor.
| 4.2 | Qualified Medical Child Support Orders. |
(a) To
the extent provided by applicable law, the Plan Administrator will extend health benefits coverage under the Plan to the person or persons
named in a qualified medical child support order, as defined in Section 609 of ERISA, as determined pursuant to such procedures regarding
qualified medical child support orders as the Plan Administrator will from time to time adopt (“QMCSO Procedures”). The QMCSO
Procedures are incorporated by reference herein.
(b) The
Plan Administrator will have the right to amend the QMCSO Procedures, as provided therein.
(c) A
participant may obtain a copy of the QMCSO Procedures free of charge upon request to the Plan Administrator.
ARTICLE 5
ADMINISTRATION OF THE PLAN
5.1 Named
Fiduciary. The Company (or the Committee, if so appointed pursuant to Section 5.5) will have all the duties and liabilities
assigned to it as “Named Fiduciary” under Section 402 of ERISA. The Named Fiduciary will have the exclusive right,
power, and authority, in its sole and absolute discretion, to administer, apply and interpret the Plan and any other Plan documents
and to decide all matters arising in connection with the operation or administration of the Plan. The Named Fiduciary may designate
such persons as appropriate to administer the Plan on a daily basis. Without limiting the generality of the foregoing, the Named
Fiduciary will have the sole and absolute discretionary authority:
(b) To
take all actions and make all decisions with respect to the eligibility for, and the amount of, benefits payable under the Plan;
(c) To
formulate, interpret and apply rules, regulations and policies necessary to administer the Plan in accordance with its terms;
(d) To
decide questions, including legal or factual questions, relating to the calculation and payment of benefits under the Plan;
(e) To
resolve and/or clarify any ambiguities, inconsistencies and omissions arising under the Plan or other Plan documents; and
(f) Except
as provided to the contrary under the Plan and applicable law, to process, and approve or deny, benefit claims and rule on any benefit
exclusions.
All determinations made by the Named
Fiduciary (or its designee) with respect to any matter arising under the Plan and any other Plan documents will be final and binding
on all parties. If any such determination will involve a question of law, the Named Fiduciary (or its designee) may rely and act
upon the advice of legal counsel with respect thereto. Pursuant to this Section 5.1, the Named Fiduciary may delegate its
discretionary authority to the Committee described in Section 5.5 of the Plan. In such case, the Committee will possess the
Named Fiduciary’s discretionary authority set forth in this Section 5.1.
Without limiting the generality of the foregoing,
if the HRA Accounts are provided through or administered by a third-party recordkeeper, that recordkeeper may be considered the Named
Fiduciary and will have the sole and absolute discretionary authority as described above. You will be notified if that is the case.
| 5.2 | Allocation of Responsibilities. |
(a) The
Company may allocate certain of its fiduciary responsibilities to one or more other persons and/or designate other persons to carry out
certain of its fiduciary responsibilities in accordance with and subject to the limitations of Section 405 of ERISA. Any person
or group of persons may serve in more than one fiduciary capacity with respect to the Plan. The Company and any fiduciary designated
by the Company may employ one or more persons to render advice with respect to their responsibilities under the Plan. The Company will
appoint a claims administrator (“Claims Administrator”) to authorize payment of claims under the Plan.
(b) The
Company, acting through its Human Resources Department, has the responsibility for the day-to-day ministerial administration of the Plan,
including any reporting obligations under applicable law. The Company may engage third parties to assist in such tasks and may delegate
to them responsibility for the tasks for which each party was so engaged. If the Company engages a third-party administrator to administer
claims under the Plan, references in this document to the Human Resources Department will be construed, as applicable, to be references
to such third-party administrator.
5.3 Liability
for Allocated Responsibilities. Neither the Company nor any other fiduciary will be liable for an act or omission of another
person in carrying out any fiduciary responsibility where such fiduciary responsibility is or may be allocated to such other person
by the Plan or pursuant to a procedure established by the Plan except to the extent provided under ERISA.
5.4 Actions
of the Company to be Uniform; Regular Personnel Policies to be Followed. Any discretionary actions to be taken under this Plan by
the Company with respect to the classification of the retirees, contributions or benefits will be uniform in their nature and applicable
to all retirees similarly situated. With respect to service with the Company, leaves of absence and other similar matters, the Company
will administer the Plan in accordance with the Company’s regular personnel policies at the time in effect.
5.5 Committee.
The Committee is responsible for the administrative and/or fiduciary responsibilities to which it is delegated by the Company. The members
of the Committee will be appointed by the Company. The Committee may delegate any of its powers or responsibilities to one or more persons
as provided in Section 5.7 below and, in such case, applicable references in this document to the Committee will be considered to
be references to such delegate.
5.6 Decisions
of Committee are Binding. The decisions of the Committee (or its delegate) with respect to any matter on which it is empowered to
act will be made in the sole discretion of the Committee and will be final, conclusive and binding on all persons, based on the Plan and,
to the extent applicable, the governing documents for any component of the Plan. In carrying out its functions under the Plan, the Committee
will endeavor to act by general rules so as to administer the Plan in a uniform and nondiscriminatory manner as to all persons similarly
situated.
5.7 Delegation
of Authority. The Committee may delegate any and all of its powers and responsibilities hereunder to other persons who may be
employees. Any such delegation may be made in writing or orally, as determined by the Committee, in its discretion; provided,
however, that no delegation will be effective until it is accepted by the persons so designated and any such delegation may be
rescinded at any time by written or oral notice from the Committee, in its discretion, to the person to whom the delegation is made.
Notwithstanding any other provision to the contrary, the Committee delegates to each insurance company the responsibility for
administering the respective component of the Plan, if any, provided through such insurance company and for exercising other
fiduciary functions described in that component of the Plan. The Committee will retain all fiduciary responsibility with respect to
the administration of the components of the Plan that the Committee has not delegated to an insurance company.
5.8 Reliance
on Various Documents. The members of the Committee, the Plan Administrator, the Employers and their respective officers,
employees (including “leased employees”) and directors will be entitled to rely upon all tables, valuations,
certificates and reports furnished by the Plan consultant selected by the Company, upon all certificates and reports made by any
accountant selected by the Committee and upon all opinions given by any legal counsel selected by the Company. The members of the
Committee, the Plan Administrator, the Employers and their respective officers, employees and directors will be fully protected in
respect of any action taken or suffered by them in good faith in reliance upon any such consultant, accountant or counsel, and all
action so taken or suffered will be conclusive upon all parties.
5.9 Accounts
and Records. The Plan Administrator will maintain such accounts and records regarding the fiscal and other transactions of the
Plan and such other data as may be required to carry out its functions under the Plan and to comply with all applicable laws. The
Plan Administrator will report to the Company’s Board of Directors (the “Board”) on the financial condition
and administrative operation of the Plan at such times as requested by the Board. The fiscal records of the Plan will be maintained
on the basis of the Plan Year.
5.10 Compliance
with Applicable Law. The Company will be deemed the Plan Administrator for the purposes of any applicable law and will be
responsible for the preparation and filing of any required returns, reports, statements or other filings with appropriate
governmental agencies. The Company will also be responsible for the preparation and delivery of information to persons entitled to
such information under any applicable law.
5.11 Liability.
The functions of the Committee and the Plan Administrator under the Plan are fiduciary in nature and each will be carried out solely in
the interest of the participants and other persons entitled to benefits under the Plan for the exclusive purpose of providing the benefits
under the Plan (and for the defraying of reasonable expenses of administering the Plan). The Committee and the Plan Administrator will
carry out their respective functions in accordance with the terms of the Plan with the care, skill, prudence and diligence under the circumstances
then prevailing that a prudent person acting in a like capacity and familiar with such matters would use in the conduct of an enterprise
of a like character and with like aims. No member of the Committee, or any officer, director or employee of the Plan Administrator or
the Employers (or any of their affiliates) will be liable for any action or inaction with respect to his or her functions under the Plan
unless such action or inaction is adjudicated to be a breach of the fiduciary standard of conduct set forth above. Further, no member
of the Committee will be personally liable merely by virtue of any instrument executed by him or her or on his or her behalf as a member
of the Committee.
5.12 Indemnification.
The Employers will, to the fullest extent permitted by law and the certificate of incorporation, by-laws, or other governing documents
of the Employers, and to the extent not covered by insurance, indemnify each director, officer or employee of the Employers and each member
of the Committee against all expenses, costs, liabilities and losses (including attorneys’ fees, judgments, fines, excise taxes
or penalties under ERISA or otherwise and amounts paid or to be paid in settlement) actually and reasonably incurred by such person in
connection with any threatened, pending or actual suit, action or proceeding (whether civil, criminal, administrative or investigative
in nature or otherwise) in which such person may be involved by reason of the fact that he or she is or was serving this Plan in any capacity,
including as a fiduciary, at the request of the Company or of another Employer, except in instances where any such person engages in gross
negligence or willful misconduct. Such right of indemnification will include the right to be paid by the Employers for expenses incurred
or reasonably anticipated to be incurred in defending any such suit, action or proceeding in advance of its disposition; provided,
however, that the payment of expenses in advance of the settlement or final disposition of a suit, action or proceeding will be made only
upon delivery to the Employers of an undertaking by or on behalf of such person to repay all amounts so advanced if it is ultimately determined
that such person is not entitled to be indemnified hereunder.
5.13 Claims
Procedure. Claims will be governed by the claim procedures pursuant to the terms of the applicable component of the Plan. To the extent
claims procedures are not set forth in separate governing documents for the respective component of the Plan, the claims procedures set
forth below will apply. The claims procedures set forth in Section 5.14 are intended to comply with United States Department of Labor
Regulation §2560.503-1 and should be construed in accordance with such regulation. In no event will Section 5.14 be interpreted
as expanding the rights of claimants beyond what is required by Regulation §2560.503-1.
| 5.14 | Initial Claims and Review Procedures. |
(a) Initial
Claims. If you or another possible payee (the “Claimant”) are seeking any benefit under this Plan, the Claimant may file
a claim with the Company’s Human Resources Department (or a third-party administrator if such information has been communicated
to Plan participants), as specified in (i) and (ii) below. The Company’s Human Resources Department or the third-party
administrator, as applicable, will review the claim itself or appoint an individual or an entity to review the claim on its behalf.
(i) Death
Benefit and Eligibility Claims. In the case of a claim for a death benefit or from an individual with regard to his or her
status as an Eligible Retiree, the Claimant will be notified within 90 days after the claim is filed whether the claim is allowed or
denied, unless the Claimant receives written notice from the Company’s Human Resources Department prior to the end of the
90-day period stating that special circumstances require an extension of the time for decision, such extension not to extend beyond
the day which is 180 days after the day the claim is filed.
(ii) Health
Benefit Claims. The Company’s Human Resources Department or the third-party administrator, as applicable, will notify the
Claimant of the Plan’s benefit determination within a reasonable period of time, but not later than 30 days after receipt of
the claim. If, due to matters beyond the control of the Plan, the Company’s Human Resources Department or the third-party
administrator, as applicable, needs additional time to process a claim, the Claimant will be notified, within 30 days after receipt
of the claim, of those circumstances and of when the Company’s Human Resources Department or the third-party administrator, as
applicable, expects to make its decision. Under no circumstances may the time for making its decision extend beyond 45 days after
receiving the claim. However, if such a delay is necessary due to the failure of the Claimant to submit the information necessary to
decide the claim, the notice of extension will specifically describe the required information, and the Claimant will be afforded at
least 45 days from receipt of the notice within which to provide the specified information.
(iii) Calculation
of Time Periods. For purposes of the time periods specified in this Section, the period of time during which a benefit determination
is required to be made begins at the time a claim is filed in accordance with the Plan procedures without regard to whether all the information
necessary to make a decision accompanies the claim. If a period of time is extended due to a Claimant’s failure to submit all information
necessary, the period for making the determination will be tolled from the date the notification is sent to the Claimant until the earlier
of: (1) date the Claimant responds, or (2) expiration of the 45-day period within which the Claimant must provide the requested
additional information.
(iv) Manner
and Content of Denial of Initial Claims. If the Company’s Human Resources Department or the third-party administrator, as applicable,
denies a claim, it must provide to the Claimant, in writing or by electronic communication:
(A) The
specific reasons for the denial or other adverse benefit determination;
(B) A
specific reference to the pertinent Plan provision or other authority upon which the denial is based;
(C) A
description of any additional information or material that the Claimant must provide in order to perfect the claim;
(D) An
explanation of why such additional material or information is necessary;
(E) Notice
that the Claimant has a right to request a review of the claim denial and information on the steps to be taken and the applicable time
limits if the Claimant wishes to request a review of the claim denial; and
(F) A
statement of the Claimant’s right to bring a civil action under Section 502(a) of ERISA following a denial on review of
the initial denial.
In addition, in
the case of a denial with respect to the HRA, the following must be provided:
(G) A
copy of any internal rule, guideline, protocol, or other similar criterion relied upon in making the adverse determination or a statement
that the same will be provided upon request by the Claimant and without charge; and
(H) If
the adverse determination is based on medical necessity, experimental treatment or similar exclusion or limit, either an explanation of
the scientific or clinical judgment applying the exclusion or limit to the Claimant’s medical circumstances or a statement that
the same will be provided upon request by the Claimant and without charge.
(i) Death
Benefit and Eligibility or Eligible Dependent Claims. A request for review of a denied claim must be made in writing to the
Committee within 60 days after receiving notice of the denial. The decision upon review will be made within 60 days after the
Committee’s receipt of a request for review, unless special circumstances require an extension of time for processing, in
which case a decision will be rendered not later than 120 days after receipt of a request for review. A notice of such an extension
must be provided to the Claimant within the initial 60-day period and must explain the special circumstances and provide an expected
date of decision.
The Committee will afford the Claimant
an opportunity to review and receive, without charge, all relevant documents, information and records and to submit issues and comments
in writing to the Committee. The Committee will take into account all comments, documents, records and other information submitted by
the Claimant relating to the claim regardless of whether the information was submitted or considered in the initial benefit determination.
A document, record or other information
is considered “relevant” to a claim for this purpose if it: (i) was relied upon in making the benefit determination,
(ii) was submitted, considered or generated in the course of making the benefit determination, without regard to whether such document,
record or other information was relied upon in making the benefit determination, or (iii) demonstrates compliance with the administrative
process and safeguards required by law when making the benefit determination.
(ii) Health
Benefit Claims. In addition to having the right to review documents and submit comments as described in (b)(i) above, a Claimant
will have at least 180 days following receipt of a notification of an adverse benefit determination of a claim for health benefits to
request a review of the initial determination. In such cases, the review will meet the following requirements:
(A) The
Plan will provide a review that does not afford deference to the initial adverse benefit determination and that is conducted by an appropriate
fiduciary of the Plan who did not make the initial determination that is the subject of the appeal, nor is a subordinate of the individual
who made the determination.
(B) The
appropriate fiduciary of the Plan will consult with a health care professional who has appropriate training and experience in the field
of medicine involved in the medical judgment before making a decision on review of any adverse initial determination based in whole or
in part on a medical judgment, including determinations with regard to whether a particular treatment, drug or other item is experimental,
investigational or not medically necessary or appropriate. The professional engaged for purposes of a consultation in the preceding sentence
will be an individual who was neither an individual who was consulted in connection with the initial determination that is the subject
of the appeal, nor the subordinate of any such individual.
(C) The
Plan will identify to the Claimant the medical or vocational experts whose advice was obtained on behalf of the Plan in connection with
the review, without regard to whether the advice was relied upon in making the benefit review determination.
(iii) Deadline
for Review Decisions. The Committee will notify the Claimant of the Plan’s benefit determination on review within a reasonable
period of time, but in no event later than 60 days after receipt by the Plan of the Claimant’s request for review of the initial
adverse determination.
(iv) Calculation
of Time Periods. For purposes of the time periods specified in this Section 5.14, the period of time during which a benefit determination
is required to be made begins at the time a claim is filed in accordance with the Plan procedures without regard to whether all the information
necessary to make a decision accompanies the claim. If a period of time is extended due to a Claimant’s failure to submit all information
necessary, the period for making the determination will be tolled from the date the notification requesting the additional information
is sent to the claimant until the earlier of: (1) the date the Claimant responds, or (2) expiration of the 45-day period within
which the Claimant must provide the requested additional information.
(v) Manner
and Content of Notice of Decision on Review. Upon completion of its review of an adverse initial claim determination, the Committee
will provide the Claimant, in writing or by electronic notification, a notice containing:
(A) Its decision;
(B) The
specific reason or reasons for the decision, with references to the pertinent Plan provisions or insurance contract provisions on which
its decision is based;
(C) A
statement that the Claimant is entitled to receive, upon request and without charge, reasonable access to, and copies of, all documents,
records and other information relevant to the Claimant’s claim for benefits; and
(D) A
statement describing the Claimant’s right to bring a civil action under Section 502(a) of ERISA;
In addition, in
the case of a denial of benefits under the HRA, the following must be provided:
(E) If
an internal rule, guideline, protocol or other similar criterion was relied upon in making the adverse determination on review, a statement
that a copy of the internal rule, guideline, protocol or other similar criterion will be provided without charge to the Claimant upon
request;
(F) If
the adverse determination on review is based on a medical necessity, experimental treatment or similar exclusion or limit, either an explanation
of the scientific or clinical judgment on which the determination was based, applying the terms of the Plan to the Claimant’s medical
circumstances, or a statement that such an explanation will be provided without charge upon request; and
(G) The
following statement “You and your Plan may have other voluntary alternative dispute resolution options, such as mediation. One way
to find out what may be available is to contact your local U.S. Department of Labor Office and, if your benefit is an insured benefit,
your State insurance regulatory agency.”
(vi) Failure
of Plan to Follow Procedures. If the Plan fails to follow the claims procedures required by this Section 5.14, a Claimant will
be deemed to have exhausted the administrative remedies available under the Plan and will be entitled to pursue any available remedy under
Section 502(a) of ERISA on the basis that the Plan has failed to provide a reasonable claims procedure that would yield a decision
on the merits of the claim.
(vii) Failure
of Claimant to Follow Procedures. A claimant must timely file, as provided in Section 5.16, a claim for benefits and must exhaust
the Plan’s claims review procedures before filing an action in court making a claim for benefits.
5.15 Benefits.
Benefits under the Plan will be paid only if the Committee or its delegate decides, in its sole discretion, that the applicant is entitled
to them.
5.16 Limitations
Period. No claim regarding an error in the amount of a contribution or debit to an Eligible Retiree’s HRA account may be made
more than one (1) year after an account statement relating to the period in which such error allegedly occurred was issued to the
Eligible Retiree (or, in case of the Eligible Retiree’s death, to his or her successor in interest). No claim for reimbursement
or claim regarding an error in processing (or failure to process) a claim for reimbursement investment instructions may be made more than
one (1) year after the expense in question was incurred. If a claimant fails to timely file a request for reimbursement or for an
initial review as provided in the preceding sentences, or for an appeal according to the procedures outlined in Section 5.14, such
claimant will have no rights of review and will have no right to bring action (whether at law, in equity or otherwise) in any court, and
the denial of the claim will become final and binding on all persons for all purposes. No action (whether at law, in equity or otherwise)
will be commenced seeking judicial review of an adverse determination under Section 5.14 later than one (1) year after the date
of the notice of the adverse determination on which judicial review is sought, provided that the Plan will object to any attempt to seek
judicial review unless the claimant has timely filed an initial claim under this Section 5.16 and an administrative appeal under
Section 5.14.
5.17 Venue.
All proceedings arising out of or relating to this Plan must be commenced and prosecuted in a federal court in New York County, New York.
Each Participant, claimant or other person consents and submits to the non-exclusive personal jurisdiction of any federal court in New
York County, New York in respect of any such proceeding. Each Participant, claimant or other person consents to service of process upon
him or her with respect to any such proceeding by registered mail, return receipt requested, and by any other means permitted by applicable
law.
5.18 Electronic
Administration. For purposes of the Plan, any forms, elections, regulations, rules, notices and disclosure of information may, to
the extent permitted by the Committee or the Company’s Human Resources Department, as applicable, and by applicable law, be made
or provided by paper, telephonic or electronic means.
ARTICLE 6
AMENDMENT AND TERMINATION
6.1 Amendment
and Termination. The Company will have the right to modify, amend, or terminate the Plan at any time and for any reason, in its sole
and absolute discretion. The Company may amend or terminate the Plan or any component of the Plan, including any contracts, certificates
or other documents describing the programs or benefits provided under the Plan, at any time and for any reason, in its sole and absolute
discretion.
6.2 Effect
of Amendment or Termination. Any amendment or termination of the Plan or any component of the Plan will be effective as of such date
as the Company will determine except that no amendment or termination will be retroactive if contrary to applicable law.
6.3 Plan Termination and Liquidation. Notwithstanding anything to the contrary in the Plan, the Plan shall terminate as of December 31, 2024 (the “Termination Effective Date”), and no further amounts shall be deferred under the Plan after such date. Each Participant’s accrued and unpaid benefits (determined on a present value basis through age 65) shall be paid to such Participant in a single lump sum payment as soon as administratively practicable following the one-year anniversary of the Termination Effective Date, but in no case later than twenty-four (24) months after the Termination Effective Date, provided that benefits payable under the Plan prior to the liquidation date if no action had been taken to terminate the Plan shall be paid in accordance with their original schedule. This paragraph shall be construed and interpreted in a manner to comply with the requirements of Treasury Regulation section 1.409A-3(j)(4)(ix)(C).
ARTICLE 7
MISCELLANEOUS
7.1 Funded
Status of Plan. At the discretion of the Company, this Plan or any component of the Plan may be fully or partially insured, self-insured,
funded under a trust (including, where applicable, one or more trusts meeting the requirements of Code Section 501(c)(9)) or other
vehicle or unfunded, and may be contributory or noncontributory. Nothing contained in the Plan will give any employee, former employee,
retiree or any other person any right, title or interest in any property of the Company other than as a general creditor.
7.2 Prohibition
of Discrimination. Any discretionary acts to be taken under the terms and provisions of this Plan by the Plan Administrator will be
uniform in their nature and in their application to all those similarly situated, and no discretionary acts will be taken that would be
discriminatory under the provisions of the Code relating from time to time to welfare plans.
7.3 Exclusive
Benefit. All contributions to the Plan will be used for the exclusive purposes of providing benefits for participants and their eligible
beneficiaries and for defraying the reasonable expenses of administering the Plan.
| 7.4 | Restriction Against Assignment. |
(a) It
is a condition of the Plan, and all rights of each participant and beneficiary will be subject thereto, that no right or interest of
any participant or beneficiary in the Plan and no benefit payable under the Plan will be subject in any manner to anticipation,
alienation, sale, transfer, assignment, pledge, encumbrance or charge, and any action by way of anticipating, alienating, selling,
transferring, assigning, pledging, encumbering or charging will be void and have no effect; nor will any such right, interest or
benefit be in any manner liable for or subject to the debts, contracts, liabilities, engagements or torts of the person entitled to
such right, interest or benefit, except as specifically provided in this Plan or any component of the Plan. Notwithstanding the
foregoing, a participant or beneficiary may request that, in the discretion of the Plan Administrator, a reimbursement for a benefit
that is covered under the Plan that he or she has a right to receive, instead be paid to a qualified healthcare provider who has
provided the services for which such reimbursement is claimed. Where benefits are paid directly to a doctor, hospital or other
provider of care (other than to a state Medicaid agency), such direct payments are provided in the discretion of the Plan
Administrator as a convenience to the participant or beneficiary and do not imply an enforceable assignment of Plan benefits or the
right to receive such benefits. If there is any dispute as to whether a request made pursuant to this
Section 7.4(a) should be honored, the Named Fiduciary’s decision will be final, binding and conclusive on all
affected parties.
(b) Participation
in the Plan or any component of the Plan may be waived by an Eligible Retiree, provided that no term, condition or provision of the Plan
will be deemed waived unless the purported waiver is in a writing signed by the party to be charged. No written waiver will be deemed
a continuing waiver unless so specifically stated in the writing or in the Plan, and such waiver will operate only as to the specific
term, condition, or provision waived.
7.5 No
Vested Interest. No person will have any right, title or interest in the assets of the Company or any of its affiliates because of
the Plan.
7.6 Action
to Comply with Law. If the Plan Administrator determines, before or during the Plan Year, that the Plan may fail to satisfy for such
Plan Year any nondiscrimination requirement imposed by the Code or any limitation on benefits, the Plan Administrator will take such action
as the Plan Administrator deems appropriate, under rules uniformly applicable to similarly situated participants, to assure compliance
with such requirement or limitation. Such action may include, without limitation, a modification of elections with respect to those persons
or groups of persons affected by the nondiscrimination requirements or limitations on benefits, and the affected participants will be
deemed to consent to such action by reason of accepting any benefit hereunder.
7.7 Subrogation.
If you or your Eligible Dependents are injured as a result of the negligence or other wrongful acts of a third party, and you or your
Eligible Dependents apply to the Plan for benefits and receive such benefits, the Plan will then have a contractual lien on the proceeds
of any compromise, settlement, judgment and/or verdict that you or your Eligible Dependents receive from either the third party or his
insurance carrier, up to the full amount of the benefits that are paid to you and/or your Eligible Dependents by the Plan.
The Plan’s lien arises through operation
of the Plan; no additional reimbursement agreement is necessary. However, the Plan may require a retiree or his attorney to execute documents
confirming the rights of the Plan. In exchange for receiving benefits under the Plan in these situations, the retiree agrees to reimburse
the Plan the full amount of benefits that are paid to him and his Eligible Dependents from the proceeds of any such compromise, settlement,
judgment and/or verdict (to the extent permitted by law), to provide the Plan with an assignment of benefits, to file with the third party
and the court such assignments, and not to prejudice the Plan’s rights in any manner.
Except where mandated by a statute that is not
preempted by ERISA, the lien will not be reduced by any attorney fees, court costs or disbursements that you might incur in your action
to recover from the third party, and these expenses may not be used to offset your obligation to reimburse the Plan for the full amount
of the lien. Further, you agree that any recovery will not be reduced by, and is not subject to, the application of the common fund doctrine
for the recovery of attorney fees.
Should you seek to recover any monies from
the third party that caused the injuries, you must give notice to the Plan Administrator within ten (10) days after either you
or your attorney first attempts to recover such monies, and if litigation is commenced, you are required to give notice to the Plan
Administrator of any pretrial conferences within five (5) days of the same. Representatives of the Plan reserve the right to
attend such pretrial conference.
By applying for benefits under the Plan, you
agree that the proceeds of any compromise, settlement, judgment and/or verdict received from the third party, the insurance carrier
and/or any other party settling on the third party’s behalf, if paid directly to the retiree or Eligible Dependent, will be
held by you or by your Eligible Dependent in constructive trust for the Plan. The receipt of such monies makes you or your Eligible
Dependent a fiduciary of the Plan with respect to such monies and therefore subject to the fiduciary provisions and obligations of
ERISA. By applying for and receiving benefits from the Plan in such third party situations, you agree to restore to the Plan the
full amount of the benefits that are paid to you and/or your Eligible Dependents from the proceeds of any such compromise,
settlement, judgment and/or verdict, to the extent permitted by law.
By accepting benefits from the Plan, you agree
to timely comply with any and all requests from the Plan for documentation concerning any legal proceedings, settlement negotiations and/or
medical information that may give rise to or affect the Plan’s right to subrogation and/or restitution.
The Plan does not require you to seek any recovery
whatsoever against the third party, and if you do not receive any recovery from the party, you are not obligated in any way to reimburse
the Plan for any of the benefits that you applied for and accepted.
In the event that you fail to notify the Plan as
provided for above, and/or fail to restore the Plan such funds as provided for above, the Plan reserves the right, in addition to all
other remedies available to it at law or equity, to withhold any other monies that might be due to you from the Plan for past or future
claims, until such time as the Plan’s lien is discharged and/or satisfied.
Any and all amounts received from a third
party by judgment, settlement, or otherwise, must be applied first to satisfy your restitution obligation to the Plan for the amount
of expenses paid by the Plan on behalf of yourself or your Eligible Dependent. The Plan’s lien is a lien of first priority for
the entire recovery of funds paid on your or your Eligible Dependent’s behalf. Where the recovery from the third party is
partial or incomplete, the Plan’s right to restitution takes priority over the your or your Eligible Dependent’s right
of recovery, regardless of whether or not you or your Eligible Dependent has been made whole for your injuries or losses. The Plan
does not recognize and is not bound by any application of the “make whole” doctrine.
7.8 Coverage
and Military Duty in the U.S. Armed Forces. If you enter the Armed Forces of the United States, you will be offered the opportunity
to continue health coverage under the Plan for yourself and for your eligible Spouse, to the extent required by the Uniformed Services
Employment and Reemployment Rights Act of 1994 (“USERRA”). If USERRA’s continuation coverage provisions apply, the Plan
will apply the same relief and funding program rules as apply under COBRA.
7.9 Women’s
Health and Cancer Rights Act. Solely to the extent required by the Women’s Health and Cancer Rights Act, the Plan will provide
certain benefits related to benefits received in connection with mastectomy. Specifically, if you receive benefits in connection with
a mastectomy under the Plan, you are also covered for the following benefits, which you may elect in consultation with your attending
physician:
| · | reconstruction of the breast on which the mastectomy has been performed; |
| · | surgery and reconstruction of the other breast to produce a symmetrical appearance; and |
| · | prosthesis and treatment of physical complications from all stages of mastectomy, including lymphedemas. |
These coverages are subject to applicable contributions
and deductibles as are consistent with those established for other medical benefits available to you under the Plan.
7.10 Newborns’
and Mothers’ Health Protection Act. In accordance with applicable law, the Plan will not restrict benefits for any
hospital length of stay in connection with childbirth for the mother or newborn child to a period of less than 48 hours following a
vaginal delivery, or less than 96 hours following a cesarean section. A provider may, however, after consulting with the mother,
discharge the mother or her newborn earlier than 48 hours (or 96 hours as applicable). In any case, the Plan and any insurance
carrier may not require that a provider obtain authorization from the Plan or insurance carrier for prescribing a length of stay not
in excess of 48 hours (or 96 hours, as applicable).
7.11 Titles
and Headings. The titles and headings of the sections of this instrument appear for convenience of reference only, and in the case
of any conflicts, the text of this instrument, rather than the titles or headings, will control.
7.12 Applicable
Law. This Plan will be construed, regulated and administered in accordance with the Code and ERISA, and to the extent not preempted
by ERISA, in accordance with the laws of the State of New York. The Plan is intended to be a welfare plan under §2510.3-1 of the
Department of Labor Regulations under ERISA, and will be construed and operated accordingly.
7.13 Conflicts.
In the event of a conflict between this document and any other Plan document, the provisions contained in this document will govern.
7.14 PBGC.
The Plan is intended to be a welfare benefit plan under ERISA and the benefits provided hereunder are not guaranteed by the Pension Benefit
Guaranty Corporation.
ARTICLE 8
HIPAA INFORMATION
8.1 HIPAA
Privacy Provisions. In fulfillment of the requirements of the privacy rule under Health Insurance Portability and
Accountability Act of 1996, P.L. 104-191, and applicable guidance (the “Privacy Rule”), 45 C.F.R.
§164.504(f)(2), the following provisions apply to the Plan constituting “group health plans,” within the meaning of
Section 607(1) of ERISA, maintained under this Plan that are subject to the Privacy Rule and that provide, or pay the
cost of, medical care and include the plans and arrangements listed in 45 C.F.R. §160.103, but only if the Company or its
affiliates have access to Protected Health Information (“PHI”), including electronic PHI. For purposes of
defining PHI, “genetic information,” within the meaning given in Section 2791 of the Public Health Services Act, as
amended by the Genetic Information Nondiscrimination Act of 2008, will be treated as health information. If the Company or an
affiliate has adopted a HIPAA privacy policy (the “Privacy Policy”) which sets forth the privacy policies and
procedures applicable to the group health plan components of the Plan: (i) the terms of the Privacy Policy, as amended from
time to time, are hereby incorporated by reference; (ii) any defined terms used herein will have the meaning given to them in
the Privacy Policy; and the provisions of this Article 8 are to be interpreted and administered consistent with the Privacy
Policy.
(a) Consistent
with the Privacy Rule, only Permitted Employees those persons holding positions with the Employers or their affiliates, as identified
in paragraph (b) below, will be permitted access to individually identifiable health information of group health plans’ participants
or beneficiaries deemed PHI under the Privacy Rule. Such persons will be restricted in their use and disclosure of PHI to Plan administrative
purposes such as those described as “payment” and “health care operations” under the Privacy Rule.
(b) Only
employees in the Company’s Human Resources Department and members of the Committee (collectively, the “Permitted
Employees”) will be given access to the PHI. Despite the foregoing, any employee or person not described above who
receives PHI relating to payments under, health care operations of, or other matters pertaining to the Plan in the ordinary course
of business, will also be included in the definition above of Permitted Employees.
(c) Reporting
Disclosures of PHI: Retirees, participants or beneficiaries of the Plan with knowledge that:
(i) employees
of the Company or its affiliates, other than Permitted Employees, have used or disclosed PHI;
(ii) Permitted
Employees have used or disclosed PHI outside the scope of Plan administration; or
(iii) employees
of the Company or its affiliates have acted contrary to the Company covenants described below,
may report such non-conforming activity to the Plan’s Privacy
and Security Officer, as identified in the Plan’s Notice of Privacy Practices, who will work with appropriate Plan and Company personnel
to correct the breach or deficiency, mitigate the effect of the breach or deficiency and impose appropriate disciplinary sanctions.
| (d) | In accordance with the certification requirement of the Privacy Rule, 45 C.F.R. §164.504(f)(2)(ii), the Company hereby certifies that it will: |
(i) Not
use or further disclose the information other than as permitted or required by the Plan documents or as required by law;
(ii) Ensure
that any agents, including subcontractors, to whom it provides PHI received from the Plan agree to the same restrictions and conditions
that apply to the Plan Sponsor with respect to such information;
(iii) Not
use or disclose the PHI for employment-related actions and decisions or in connection with any other benefit or employee benefit plan
of the Plan Sponsor;
(iv) Report
to the Plan any use or disclosure of the PHI that is inconsistent with the uses or disclosures permitted by the Privacy Rule of which
it becomes aware;
(v) Make
available PHI based on HIPAA’s access requirements in accordance with 45 C.F.R. §164.524;
(vi) Make
available PHI for amendment and incorporate any amendments to PHI in accordance with 45 C.F.R. §164.526;
(vii) Make
available the information required to provide an accounting of disclosures in accordance with 45 C.F.R. §264.528;
(viii) Make
its internal practices, books and records relating to the use and disclosure of PHI received from the Plan available to the Secretary
of Health and Human Services for purposes of determining compliance by the Plan with the Privacy Rule;
(ix) If
feasible, return or destroy all PHI received from the Plan that the Plan Sponsor still maintains in any form and retain no copies of such
information when no longer needed for the purpose for which disclosure was made, except that, if such return or destruction is not feasible,
limit further uses and disclosures to those purposes that make the return or destruction of the information infeasible; and
(x) Ensure
that adequate separation of the Plan and the Plan Sponsor is established as required by 45 C.F.R. §164.504(f)(2)(iii).
| 8.2 | HIPAA Security Provisions. |
(a) There
are some special rules under HIPAA related to “electronic protected health information.” Electronic protected health
information is generally PHI that is transmitted by, or maintained in, electronic media. “Electronic media” includes electronic
storage media, including memory devices in a computer (such as hard drives) and removable or transportable digital media (such as magnetic
tapes or disks, optical disks and digital memory cards). It also includes transmission media used to exchange information already in electronic
storage media, such as internet, an extranet (which uses internet technology to link a business with information accessible only to some
parties), leased lines, dial-up lines, private networks and the physical movement of removable/transportable electronic storage media.
(b) In
fulfillment of the requirements of the security rule under HIPAA (the “Security Rule”), 45 C.F.R. §164.314(b)(1),
the following provisions apply to the group health plans maintained under this Plan that are subject to the Security Rule and that
provide, or pay the cost of, medical care and include the plans and arrangements listed in 45 C.F.R. §160.103, but only if the Company
or its affiliates have access to electronic PHI. In such event, the Company hereby certifies that it will:
(i) Implement
administrative, physical and technical safeguards that reasonably and appropriately protect the confidentiality, integrity and availability
of the electronic PHI that it creates, receives, maintains or transmits on behalf of the Plan;
(ii) Ensure
that the adequate separation required to exist between the Plan and the Plan Sponsor is supported by reasonable and appropriate administrative,
physical and technical safeguards in its information systems;
(iii) Ensure
that any agent, including a subcontractor, to whom it provides electronic PHI agrees to implement reasonable and appropriate security
measures to protect that information;
(iv) Report
to the Plan if it becomes aware of any attempted or successful unauthorized access, use, disclosure, modification or destruction of information
or interference with system operations in its information systems; and
(v) Comply
with any other requirements that the Secretary of the U.S. Department of Health and Human Services may require from time to time with
respect to electronic PHI by the issuance of additional regulations or other guidance pursuant to HIPAA.
| 8.3 | Mitigation. In the event of non-compliance with any of the provisions set forth in this Article, |
(a) the
Plan’s Privacy and Security Officer will address any complaint promptly and confidentially. The Privacy and Security Officer first
will investigate the complaint and document his investigation efforts and findings;
(b) if
PHI has been used or disclosed in violation of the Privacy or Security Rule or inconsistent with this Section, the Privacy and Security
Officer will take immediate steps to mitigate any harm caused by the violation and to minimize the possibility that such a violation will
recur; and
(c) if
a Permitted Employee or other employee of the Company or its affiliate is found to have violated the Privacy or Security Rule, such personnel
will be subject to disciplinary action up to and including termination.
(a) Following
the discovery of a breach of unsecured PHI, a group health plan will notify each individual whose unsecured PHI has been, or is
reasonably believed to have been, accessed, acquired, or disclosed as a result of a breach, in accordance with 45 C.F.R.
§164.404, and will notify the Secretary of Health and Human Services in accordance with 45 C.F.R. §164.408. For a breach
of unsecured PHI involving more than 500 residents of a state or jurisdiction, a group health plan will notify the media in
accordance with 45 C.F.R. §164.406.
(b) For purposes of this Section 8.4,
a “breach” means the acquisition, use or disclosure of an individual’s PHI in a manner not permitted under
the Privacy Rule unless there is a low probability that the PHI has been compromised. The term “breach” does not
include:
(i) an
unintentional acquisition, access, or use of PHI by a workforce member or person acting under the authority of a covered entity or business
associate, if such acquisition, access, or use was in good faith and within the scope of authority and does not result in a further impermissible
use or disclosure;
(ii) an
inadvertent disclosure by a person who is authorized to access PHI to another person authorized to access PHI at the same covered entity
or business associate or organized health care arrangement in which the covered entity participates, and the information received is not
further used or disclosed in a manner not permitted under the Privacy Rule; or
(iii) a
disclosure of PHI where a covered entity or business associate has a good faith belief that an unauthorized person to whom the disclosure
was made would not reasonably have been able to retain such information.
(c) For
purposes of this Section 8.4, “unsecured PHI” means PHI that is not rendered unusable, unreadable or indecipherable to
unauthorized persons through the use of a technology or methodology specified in Regulations issued by the Secretary of Health and Human
Services.
(d) For
purposes of subsection (b), in determining whether there is a low probability that the PHI has been compromised, the covered entity must
make a risk assessment which considers at least the following factors:
(i) the
nature and extent of the PHI involved, including the types of identifiers and the likelihood of re-identification;
| (ii) | the unauthorized person who used the PHI or to whom the disclosure was made; |
| (iii) | whether the PHI was actually acquired or viewed; and |
| (iv) | the extent to which the risk to the PHI has been mitigated. |
ARTICLE 9
YOUR RIGHTS UNDER ERISA AND OTHER LAWS
As a participant in the plan you are entitled to
certain rights and protections under the Employee Retirement Income Security Act of 1974 (ERISA). ERISA provides that all plan
participants will be entitled to:
Receive Information About Your Plan and Benefits
| ● | You are entitled to examine, without charge, at the Plan Administrator’s office and at other specified locations, such as worksites,
all documents governing the plan, including insurance contracts, if any, and a copy of the latest annual report (Form 5500 Series)
filed by the plan with the U.S. Department of Labor and available at the Public Disclosure Room of the Employee Benefits Security Administration. |
| ● | You are also entitled to obtain, upon written request to the Plan Administrator, copies of documents governing the operation of the
plan, including insurance contracts, if any, and copies of the latest annual report (Form 5500 Series), if any, and updated summary
plan description. The Plan Administrator may make a reasonable charge for the copies. |
| ● | You may also request to receive a summary of the plan’s annual financial report. The Plan Administrator is required by law to
furnish each participant with a copy of this summary annual report. |
Continue Group Health Plan Coverage
You are entitled to continue health care coverage
for yourself, spouse or dependent child(ren) if there is a loss of coverage under the Plan as a result of a qualifying event. You or your
dependents may have to pay for such coverage. You should review this summary plan description and the documents governing the plan on
the rules governing your COBRA continuation coverage rights.
Prudent Actions by Plan Fiduciaries
In addition to creating rights for plan participants
ERISA imposes duties upon the people who are responsible for the operation of the employee benefit plan. The people who operate your plan,
called “fiduciaries” of the plan, have a duty to do so prudently and in the interest of you and other plan participants and
beneficiaries. No one, including your employer or any other person, may fire you or otherwise discriminate against you in any way to prevent
you from obtaining a benefit or exercising your rights under ERISA.
Enforce Your Rights
If your claim for a welfare benefit is denied or
ignored, in whole or in part, you have a right to know why this was done, to obtain copies of documents relating to the decision without
charge, and to appeal any denial, all within certain time schedules. Under ERISA, there are steps you can take to enforce the above rights.
For instance, if you request a copy of plan documents or the latest annual report from the plan and do not receive them within 30 days,
you may file suit in a Federal court. In such a case, the court may require the plan administrator to provide the materials and pay you
up to $110 a day until you receive the materials, unless the materials were not sent because of reasons beyond the control of the administrator.
If you have a claim for benefits which is denied or ignored, in whole or in part, you may file suit in a state or Federal court. In addition,
if you disagree with the plan’s decision or lack thereof concerning the qualified status of a domestic relations order or medical
child support order, you may file suit in Federal court. If it should happen that plan fiduciaries misuse the plan’s money, or if
you are discriminated against for asserting your rights, you may seek assistance from the U.S. Department of Labor, or you may file suit
in a Federal court. The court will decide who should pay court costs and legal fees. If you are successful, the court may order the person
you have sued to pay these costs and fees. If you lose, the court may order you to pay these costs and fees, for example, if it finds
your claim is frivolous.
Assistance with Your Questions
If you have any questions about your plan, you
should contact the plan administrator. If you have any questions about this statement or about your rights under ERISA, or if you need
assistance in obtaining documents from the plan administrator, you should contact the nearest office of the Employee Benefits Security
Administration, U.S. Department of Labor, listed in your telephone directory or the Division of Technical Assistance and Inquiries, Employee
Benefits Security Administration, U.S. Department of Labor, 200 Constitution Avenue N.W., Washington, D.C. 20210. You may also obtain
certain publications about your rights and responsibilities under ERISA by calling the publications hotline of the Employee Benefits Security
Administration.
ARTICLE 10
ADDITIONAL INFORMATION
| Plan Sponsor: |
International Seaways Ship Management, LLC
600 Third Avenue,
39th Floor
New York, NY 10016 |
| |
|
| Employer Identification Number: |
81-3657605 |
| |
|
| Plan Name: |
International Seaways Retiree Health and Welfare Plan |
| |
|
| Type of Plan: |
Welfare Benefit Plan |
| |
|
| Plan Year: |
Calendar Year |
| |
|
| Plan Number: |
501 |
| |
|
| Plan Administrator: |
International Seaways Ship Management, LLC
600 Third Avenue,
39th Floor
New York, NY 10016 |
| |
|
| Type of Administration: |
The Plan is administered by the Company. The Company generally has delegated its duties and responsibilities for administration to the Committee described in Section 5.5. |
| |
|
| Agent for Service of Legal Process: |
General Counsel
International Seaways, Inc.
c/o
International Seaways Ship Management, LLC
600 Third Avenue, 39th Floor
New York, NY 10016 |
| |
|
| Plan Funding: |
Plan benefits currently are paid from the Company’s general assets. |
| |
|
| HRA Claims |
File a claim with:
Human Resources Department
International Seaways Ship Management,
LLC
600 Third Avenue, 39th Floor
New York, NY 10016
Fax: (212) 578-1832
sstulbaum@intlseas.com |
| |
|
| Participating Employers |
International Seaways Ship Management, LLC
International Seaways, Inc. |
APPENDIX
INTERNATIONAL SEAWAYS RETIREE HEALTH AND WELFARE
PLAN
HEALTH REIMBURSEMENT ACCOUNTS
I. PURPOSE
The Health Reimbursement Arrangement accounts (“HRAs”
or “HRA accounts”) allow HRA Participants (as defined below) to obtain reimbursement of Eligible Medical Expenses (as
defined below) which are not otherwise reimbursed by any other plan or program. The HRA program is intended to qualify as a self-insured
medical reimbursement plan for purposes of Code Sections 105 and 106, as well as a health reimbursement arrangement as defined in IRS
Notice 2002-45. Reimbursements for Eligible Medical Expenses paid by the Plan generally are intended to be excludable from the HRA Participant’s
taxable income.
II. DEFINITIONS
Unless otherwise specified, terms that are capitalized
in this Appendix have the same meaning as the defined terms in the Plan. The definitions of terms defined in this Appendix, but not defined
in Section 2 of the Plan document, will be applicable only with respect to this Appendix.
2.1 Eligible
Medical Expense generally means an expense incurred by an HRA Participant for medical care as defined in Code Section 223(d)(2).
Only Eligible Medical Expenses incurred while an individual is an HRA Participant may be reimbursed from an HRA account (as defined below).
The following expenses may not be reimbursed from an HRA account:
| 1. | expenses incurred for qualified long-term care services, other than a qualified long-term care insurance contract (as defined in Code
Section 7702B(b)); |
| 2. | expenses incurred prior to the date the individual became an HRA Participant; |
| 3. | expenses incurred after the date the individual ceases to be an HRA Participant; |
| 4. | expenses paid for with pre-tax dollars; and |
| 5. | expenses that have been reimbursed (or paid directly) by another plan or for which the HRA Participant
will seek reimbursement (or direct payment) under another health plan. |
For
purposes of subsection (5), Medicare is considered another health plan.1
2.3 Eligible
Retiree means a retiree who is eligible to participate in, and has enrolled in, the Plan.
2.4 Eligible
Dependent means an Eligible Retiree’s spouse (recognized for federal tax purposes) or dependent child (under Code Section 105).
| 1 |
As a general rule, Medicare is expected to be the Primary payer for Eligible Retirees, with most claims to be only for reimbursement
of copayments and/or deductibles under Medicare, rather than for the primary amount. For the avoidance of doubt, the Company’s
liability is limited to the amount in the HRA account. |
2.5 HRA
Participant means, for purposes of this Appendix, an Eligible Retiree or an Eligible Dependent.
III. PARTICIPATION
3.1 Commencement
of Participation. An Eligible Retiree becomes an HRA Participant on the later of December 1, 2016 or the date that
he or she has first become eligible for participation under the Plan, but reimbursements will not be made until he or she has completed
any enrollment forms or procedures required by the Plan Administrator or the Company’s Human Resources Department. An Eligible Dependent
becomes an HRA Participant on the later of the date the Eligible Retiree first becomes a participant in the Plan or the date that
the dependent first becomes an Eligible Dependent of the Eligible Retiree.
| 3.2 | Cessation of Participation. |
| (a) | An Eligible Retiree will cease being an HRA Participant on the earliest of: |
| (i) | the date he or she ceases to be an Eligible Retiree for any reason; |
| (ii) | the date he or she is rehired by the Company or any of its Affiliates as an active employee; |
| (iii) | the date of his or her death; or |
| (iv) | the date the Plan, or the HRA component of the Plan, is terminated. |
(b) An
Eligible Dependent of an Eligible Retiree will cease being an HRA Participant on the earliest of:
| (i) | the date he or she ceases to be an Eligible Dependent for any reason; |
| (ii) | the date the Eligible Retiree is hired or rehired by the Company or any of its Affiliates as an active employee; |
| (iii) | the date he or she is hired or rehired by the Company or any of its Affiliates as an active employee; |
| (iv) | the date the spousal Eligible Dependent and the Eligible Retiree are divorced; |
| (v) | in the case of the spousal Eligible Dependent of an Eligible Retiree who dies, the date the spousal Eligible Dependent re-marries;
or |
| (vi) | the date the Plan, or the HRA component of the Plan, is terminated. |
(c) No
HRA Participant may obtain reimbursement of any Eligible Medical Expenses incurred after the date his or her eligibility ceases. An HRA
Participant will have until March 15 of the following year after his or her eligibility ceases, or such other period as the Plan
Administrator may determine and communicate, to request reimbursement of Eligible Medical Expenses incurred before eligibility ceased.
IV. HRA ACCOUNT
4.1 Company
Contributions The Employers each year generally will contribute the amount indicated below to the HRA account of an
Eligible Retiree, depending on the Eligible Retiree’s age on January 1 of the particular year and his or her years of
Credited Service. Contributions will cease upon the death of the retiree. Contributions for the first year of retirement will be
pro-rated based upon the number of full months in the calendar year on or after the date of retirement (e.g., 7/12 if the date of
retirement is June 1 and 6/12 if the date is June 2). An initial payment will be made as soon as feasible following
retirement and thereafter any future contributions will be made quarterly, in arrears. Similar proration will apply for the year in
which an Eligible Retiree attains age 65.
|
Years of Credited Service |
Annual Company Contributions |
| Under Age 65 |
Over Age 65 |
| 10 or less |
$1,440 |
$720 |
| 11 |
$1,728 |
$864 |
| 12 |
$2,016 |
$1,008 |
| 13 |
$2,304 |
$1,152 |
| 14 |
$2,592 |
$1,296 |
| 15 |
$2,880 |
$1,440 |
| 16 |
$3,168 |
$1,584 |
| 17 |
$3,456 |
$1,728 |
| 18 |
$3,744 |
$1,872 |
| 19 |
$4,032 |
$2,016 |
| 20 or more |
$4,320 |
$2,160 |
| (a) | The Plan Administrator will establish a notional bookkeeping account (an “HRA account”) for each Eligible Retiree
that keeps a record of amounts allocated to the Eligible Retiree’s account and reimbursements made to the Eligible Retiree or his
or her Eligible Dependents from the HRA. When the Eligible Retiree first becomes an HRA Participant, and each Plan Year thereafter while
the Eligible Retiree is alive, the Company will credit a specified amount of Employer contributions, as described above,” to the
HRA account. At the Employers’ discretion, additional contributions may be made with respect to December, 2016. Separate credits will not be made for an Eligible Retiree
and his or her Eligible Dependents. HRA Participants may not contribute to HRA accounts. |
| (b) | The amount in the HRA account will be reduced from time to time by the amount of any Eligible Medical Expenses for which the Eligible
Retiree or his or her Eligible Dependents are reimbursed under the HRA Plan. At any time, an HRA Participant may receive reimbursement
for Eligible Medical Expenses up to the amount remaining in the Eligible Retiree’s HRA account. If there are insufficient funds
credited in an HRA account to reimburse Eligible Medical Expenses, the claim for reimbursement will be held until sufficient additional
funds are credited to the HRA account. If sufficient additional funds will not be credited, reimbursement will be made to the extent of
funds remaining in the HRA account. |
| (c) | An HRA account is a bookkeeping account on the Employers’ records; it is not funded and does not bear interest or accrue earnings
of any kind. All benefits under the HRA component of the Plan are paid entirely from
the Employers’ general assets. |
4.3 Unused
Funds in HRA account. If an Eligible Retiree and his or her Eligible Dependents do not use all of the amounts credited to his
or her HRA account during a Plan Year, those amounts will be carried over for reimbursement of Eligible Medical Expenses in subsequent
Plan Years (as long as he or she remains an Eligible Retiree). Any unused funds in an HRA account will be forfeited back to the Company
upon the earlier of: (i) when neither an Eligible Retiree nor any of his or her Eligible Dependents are eligible for further
reimbursements from the HRA account or (ii) as of December 31 of the Plan Year in which the individual ceased to be an Eligible
Retiree (other than by death).
4.4 Death
of Eligible Retiree. If an Eligible Retiree dies with no Eligible Dependent, his or her HRA account is immediately forfeited
as of his or her death. If an Eligible Retiree pre-deceases his or her Eligible Dependents, his or her HRA account will be forfeited upon
the earlier of: (i) as of the death of the Eligible Dependents (or earlier, if Section 3.2(b) applies) or (ii) as
of December 31 of the Plan Year following the Plan Year in which the Eligible Retiree died. However, the deceased Eligible Retiree’s
or Eligible Dependent’s estate or representatives may submit claims for Eligible Medical Expenses incurred by the Eligible Retiree
or the Eligible Dependent before his or her death. Claims must be submitted within the period established under Section 3.2(c), based
upon the date on which the expense was incurred.
If an Eligible Retiree dies with an Eligible Dependent
who is an HRA Participant, the Eligible Dependent can continue to submit for reimbursement his or her Eligible Medical Expenses incurred
through December 31 of the Plan Year following the Plan Year in which the Eligible Retiree died.
| 4.5 | Claims for Reimbursement. |
An HRA Participant who has incurred Eligible Medical
Expenses during a period of coverage may seek reimbursement for such Eligible Medical Expenses in accordance with the following:
| (a) | Written Application: He or she may apply to the Company’s Human Resources Department for reimbursement
of Eligible Medical Expenses by submitting a written application in such form as the Human Resources Department may from time to time
prescribe, which generally must include: |
| (i) | the date and nature of the expense for which reimbursement is requested; |
| (ii) | the name, address and tax ID or Social Security number of the person, organization or entity to which
such expense was paid or is payable; |
| (iii) | a written statement (such as a bill or invoice) from an independent third party stating that such expenses
have been incurred and the amount of such expenses; |
| (iv) | a statement from the HRA Participant that such expenses have not been reimbursed and will not be reimbursed
under any other plan; and |
| (v) | such other information as the Human Resources Department may from time to time require including, but not limited to, receipts, cancelled
checks, original statements or explanation of benefit forms from a group health plan and verification of dependent, student or marital
status, and verification of disability for children over age 26. |
| (b) | Timing. Claims for reimbursement must be filed by March 15 of the year following the year in which the expense was incurred.
You will be notified if the filing deadline is changed. |
4.6 Overpayments.
If it is determined that an HRA Participant received
an overpayment or a payment was made in error (e.g., an HRA Participant was reimbursed from the HRA account for an expense that is later
paid by another medical plan), the HRA Participant will be required to refund the overpayment or erroneous reimbursement. If the overpayment
or erroneous payment is not refunded, the Plan reserves the right to offset future reimbursements equal to the overpayment or erroneous
payment or, if that is not feasible, to withhold such funds from any other amounts due under the Plan to the HRA Participant. If all other
attempts to recoup the overpayment or erroneous payment are unsuccessful, the Plan Administrator may treat the overpayment as a bad debt.
4.7 Termination
of Participation. Upon termination of participation (other than by death of the Eligible Retiree, as described in Section 4.4
of this Appendix), the operation of the HRA will depend on whether or not the HRA Participant is eligible for, and elects, continuation
coverage under COBRA.
| (a) | If COBRA is elected: If the HRA Participant is eligible for COBRA with respect to the HRA, he or she must make timely after-tax payments
of the required contributions for the period of COBRA coverage. If he or she elects COBRA and pays the applicable premiums, he or she
can submit for reimbursement any Eligible Medical Expenses incurred through the expiration of the COBRA period. Any unused amounts in
the HRA at the time participation ended will remain available to be used for Eligible Medical Expenses incurred during that period, but
no new allocations of Company amounts will occur. |
| (b) | If the HRA Participant does not elect (or is not eligible for) COBRA: Eligible Medical Expenses incurred before the termination of
participation may be reimbursed to the extent of the amount remaining in the HRA at the time of termination, but not any expenses incurred
thereafter. A request for reimbursement of Eligible Medical Expenses incurred before the termination of participation must be submitted
by March 15 of the year following the year in which the expense was incurred. |
v3.24.4
| X |
- DefinitionBoolean flag that is true when the XBRL content amends previously-filed or accepted submission.
| Name: |
dei_AmendmentFlag |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionFor the EDGAR submission types of Form 8-K: the date of the report, the date of the earliest event reported; for the EDGAR submission types of Form N-1A: the filing date; for all other submission types: the end of the reporting or transition period. The format of the date is YYYY-MM-DD.
| Name: |
dei_DocumentPeriodEndDate |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:dateItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe type of document being provided (such as 10-K, 10-Q, 485BPOS, etc). The document type is limited to the same value as the supporting SEC submission type, or the word 'Other'.
| Name: |
dei_DocumentType |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:submissionTypeItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAddress Line 1 such as Attn, Building Name, Street Name
| Name: |
dei_EntityAddressAddressLine1 |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAddress Line 2 such as Street or Suite number
| Name: |
dei_EntityAddressAddressLine2 |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Definition
+ References
+ Details
| Name: |
dei_EntityAddressCityOrTown |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionCode for the postal or zip code
| Name: |
dei_EntityAddressPostalZipCode |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionName of the state or province.
| Name: |
dei_EntityAddressStateOrProvince |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:stateOrProvinceItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionA unique 10-digit SEC-issued value to identify entities that have filed disclosures with the SEC. It is commonly abbreviated as CIK. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityCentralIndexKey |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:centralIndexKeyItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionIndicate if registrant meets the emerging growth company criteria. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityEmergingGrowthCompany |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionCommission file number. The field allows up to 17 characters. The prefix may contain 1-3 digits, the sequence number may contain 1-8 digits, the optional suffix may contain 1-4 characters, and the fields are separated with a hyphen.
| Name: |
dei_EntityFileNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:fileNumberItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTwo-character EDGAR code representing the state or country of incorporation.
| Name: |
dei_EntityIncorporationStateCountryCode |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:edgarStateCountryItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe exact name of the entity filing the report as specified in its charter, which is required by forms filed with the SEC. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityRegistrantName |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe Tax Identification Number (TIN), also known as an Employer Identification Number (EIN), is a unique 9-digit value assigned by the IRS. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityTaxIdentificationNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:employerIdItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionLocal phone number for entity.
| Name: |
dei_LocalPhoneNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true only for a security having no trading symbol.
| Name: |
dei_NoTradingSymbolFlag |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:trueItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as pre-commencement communications pursuant to Rule 13e-4(c) under the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 13e
-Subsection 4c
| Name: |
dei_PreCommencementIssuerTenderOffer |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as pre-commencement communications pursuant to Rule 14d-2(b) under the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 14d
-Subsection 2b
| Name: |
dei_PreCommencementTenderOffer |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTitle of a 12(b) registered security. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b
| Name: |
dei_Security12bTitle |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:securityTitleItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionName of the Exchange on which a security is registered. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection d1-1
| Name: |
dei_SecurityExchangeName |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:edgarExchangeCodeItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as soliciting material pursuant to Rule 14a-12 under the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Section 14a
-Number 240
-Subsection 12
| Name: |
dei_SolicitingMaterial |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTrading symbol of an instrument as listed on an exchange.
| Name: |
dei_TradingSymbol |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:tradingSymbolItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as written communications pursuant to Rule 425 under the Securities Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Securities Act
-Number 230
-Section 425
| Name: |
dei_WrittenCommunications |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Details
| Name: |
us-gaap_StatementClassOfStockAxis=us-gaap_CommonStockMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
| X |
- Details
| Name: |
us-gaap_StatementClassOfStockAxis=insw_RightscommonstockMember |
| Namespace Prefix: |
|
| Data Type: |
na |
| Balance Type: |
|
| Period Type: |
|
|
International Seaways (NYSE:INSW)
Historical Stock Chart
Von Dez 2024 bis Jan 2025
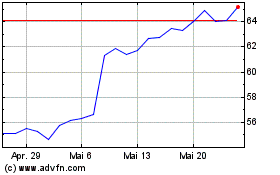
International Seaways (NYSE:INSW)
Historical Stock Chart
Von Jan 2024 bis Jan 2025