Abecma tripled progression-free survival
compared to standard regimens in the Phase 3 KarMMa-3 trial, with a
51% reduction in risk of disease progression or death and a
well-established safety profile
Expanded approval brings this personalized
CAR T cell therapy to more patients with relapsed or refractory
multiple myeloma earlier in their treatment journey as a one-time
infusion offering meaningful treatment-free intervals when
responding to therapy
Abecma is now approved in the U.S., Japan,
Switzerland and the EU for earlier use for triple-class exposed
relapsed and/or refractory multiple myeloma, underscoring BMS’
commitment to delivering Abecma globally, with consistently high
manufacturing success rates and continuous increases in
capacity
Bristol Myers Squibb (NYSE: BMY) and 2seventy bio, Inc. (Nasdaq:
TSVT) have announced that on April 4, 2024, the U.S. Food and Drug
Administration (FDA) approved Abecma® (idecabtagene vicleucel;
ide-cel) for the treatment of adult patients with relapsed or
refractory multiple myeloma after two or more prior lines of
therapy including an immunomodulatory agent (IMiD), a proteasome
inhibitor (PI), and an anti-CD38 monoclonal antibody, based on
results from the KarMMa-3 trial. This approval expands Abecma’s
indication, making it available in earlier lines to patients who
have relapsed or become refractory after exposure to these three
main classes of treatment (triple-class exposed), after two prior
lines of therapy. Abecma is administered as a one-time infusion,
with a new recommended dose range of 300 to 510 x 106 CAR-positive
T cells. Please see the Important Safety Information section below,
including Boxed WARNINGS for Abecma regarding Cytokine
Release Syndrome, Neurologic Toxicities, Hemophagocytic
Lymphohistiocytosis/Macrophage Activation Syndrome, Prolonged
Cytopenia, and Secondary Hematological Malignancies.
This press release features multimedia. View
the full release here:
https://www.businesswire.com/news/home/20240403030392/en/
Product image for download (Photo:
Bristol Myers Squibb)
“Abecma has demonstrated a progression-free survival benefit
three times that of standard regimens in relapsed or refractory
multiple myeloma, and we are now bringing the promise of cell
therapy to patients earlier in their treatment journey,” said Bryan
Campbell, senior vice president, Head of Commercial, Cell Therapy,
Bristol Myers Squibb. “This approval underpins our commitment to
addressing the unmet needs of more patients living with multiple
myeloma by improving upon the current treatment paradigm, and we
remain steadfast in our pursuit of innovation and advancing cell
therapy research to deliver potentially transformative
therapies.”
“We are extremely pleased that Abecma will be available to many
more patients in the U.S.,” said Chip Baird, chief executive
officer, 2seventy bio. “This approval represents another important
milestone for patients, for Abecma, and for 2seventy bio as we
remain committed to increasing treatment options and working to
improve outcomes for patients living with multiple myeloma.”
Despite advances in treatment, multiple myeloma remains an
incurable disease characterized by periods of remission and
relapse. In early lines of treatment, regimens consisting of
combinations of IMiDs, PIs, and anti-CD38 monoclonal antibodies are
often used to help manage the disease. Unfortunately, as many
patients go on to relapse and/or become refractory to these classes
of therapy, more patients are becoming triple-class exposed earlier
in their treatment journey. There are limited options for these
patients, and triple-class exposed relapsed and/or refractory
multiple myeloma is associated with poor outcomes and a median
progression-free survival (PFS) of three to five months. In this
patient population with high unmet need, Abecma has demonstrated
clinically meaningful and statistically significant improvements in
PFS (95% CI: 13.3 months vs. 4.4 months [HR: 0.49; p<0.0001]).
In addition, Abecma exhibited a well-established safety profile
with mostly low-grade cytokine release syndrome and neurotoxicity.
No cases of Parkinsonism were reported in the study.
“The results of the KarMMa-3 study are remarkable, especially
given the historic outcomes with standard regimens for these
patients with relapsed or refractory disease,” said Al-Ola A.
Abdallah, M.D., University of Kansas, Clinical Associate Professor,
Clinical Director, Hematologic Malignancies and Cellular
Therapeutics and chair of U.S. Myeloma Innovations Research
Collaborative. “With this approval, these patients now have an
opportunity to be treated at an earlier line of therapy with a
potentially transformative therapy that offers significantly
improved progression-free survival for this difficult-to-treat
disease that has had no established treatment approach.”
To support this approval and future expansions, Bristol Myers
Squibb has made continuous investments to increase manufacturing
capacity and has shown a consistently high manufacturing success
rate of 94% for Abecma in the commercial setting.
Abecma was recently approved in Japan, Switzerland and the
European Union for adult patients with triple-class exposed
relapsed and/or refractory multiple myeloma after two prior lines
of therapy, making it the only CAR T cell therapy available
globally for earlier lines of therapy for patients with
triple-class exposed relapsed and/or refractory multiple myeloma.
Abecma is also currently approved in Great Britain and Israel for
adult patients with triple-class exposed relapsed and refractory
multiple myeloma after three or more prior lines of therapy.
KarMMa-3 Pivotal Trial
Results
The KarMMa-3 trial is a pivotal, Phase 3, open-label, global,
randomized, controlled trial evaluating Abecma compared to standard
regimens in patients with relapsed and refractory multiple myeloma
who have received two to four prior lines of treatment, including
an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38
antibody, and were refractory to the last treatment regimen, with
94% of patients with disease refractory to prior treatment with
daratumumab. KarMMa-3 is the only Phase 3 trial to evaluate a CAR T
cell therapy in a patient population consisting entirely of
triple-class exposed relapsed and refractory multiple myeloma
patients. The trial’s patient-centric design allowed for crossover
from standard regimens to Abecma upon confirmed disease
progression. At the time of the final progression-free survival
(PFS) analysis, more than half (56%) of patients in the standard
regimens arm crossed over to receive Abecma as a subsequent
therapy.
In the study, 254 patients were randomized to receive Abecma and
132 were randomized to receive standard regimens that consisted of
combinations that included daratumumab, pomalidomide, and
dexamethasone (DPd), daratumumab, bortezomib, and dexamethasone
(DVd), ixazomib, lenalidomide, and dexamethasone (IRd), carfilzomib
and dexamethasone (Kd) or elotuzumab, pomalidomide and
dexamethasone (EPd) chosen based on their most recent treatment
regimen and investigator discretion. In the Abecma arm,
pretreatment consisted of leukapheresis and optional bridging
therapy. The choice to use bridging therapy was at the discretion
of the investigator.
At an estimated median duration of follow-up of 15.9 months at
the primary PFS analysis, Abecma more than tripled the primary
endpoint of PFS compared with standard regimens, with a median PFS
of 13.3 months (95% CI: 11.8-16.1) vs. 4.4 months (95% CI:
3.4-5.9), respectively (HR:0.49; 95% CI: 0.38-0.64; p<0.0001),
representing a 51% reduction in the risk of disease progression or
death with Abecma. Abecma also showed a significant improvement in
overall response rates (p<0.0001) with the majority (71%) of
patients treated with Abecma achieving a response, and 39%
achieving a complete or stringent complete response. In comparison,
less than half of patients (42%) who received standard regimens
achieved a response, with 5% experiencing a complete response or
stringent complete response. Responses were durable with Abecma,
with a median duration of response of 14.8 months (95% CI:
12.0-18.6). In those patients who derived a complete response or
better, median duration of response was 20 months (95% CI:
15.8-24.3).
Abecma has exhibited a well-established and consistent safety
profile with mostly low-grade cytokine release syndrome (CRS) and
neurotoxicity. Among patients who received Abecma in the KarMMa and
KarMMa-3 studies (n=349), any grade CRS occurred in 89% of
patients, including Grade >3 CRS in
7% of patients, and three cases (0.9%) of Grade 5 CRS reported. The
median time to onset of CRS was 1 day (range: 1-27 days), and the
median duration of CRS was 5 days (range: 1-63 days). Any grade
neurotoxicity occurred in 40% of patients treated with Abecma in
the KarMMa and KarMMa-3 studies, including Grade 3 neurotoxicity in
4% of patients, and two cases (0.6%) of Grade 4 neurotoxicity
reported. At the safety update for KarMMa-3, one case of Grade 5
neurotoxicity was reported. The median time to onset of
neurotoxicity was 2 days (range: 1-148 days), and the median
duration of neurotoxicity was 8 days (range: 1-720 days).
About Abecma
Abecma is a CAR T cell therapy that recognizes and binds to BCMA
on the surface of multiple myeloma cells leading to CAR T cell
proliferation, cytokine secretion, and subsequent cytolytic killing
of BCMA-expressing cells. Abecma is being jointly developed and
commercialized in the U.S. as part of a Co-Development,
Co-Promotion, and Profit Share Agreement between Bristol Myers
Squibb and 2seventy bio.
This approval further underscores Bristol Myers Squibb’s deep
knowledge and experience in cell therapy science and continued
clinical advancements for multiple myeloma patients. The companies’
broad clinical development program for Abecma includes ongoing and
planned clinical studies (KarMMa-2, KarMMa-3, KarMMa-9) for
patients with multiple myeloma. For more information visit
clinicaltrials.gov.
U.S. Important Safety
Information
BOXED WARNING: CYTOKINE RELEASE SYNDROME, NEUROLOGIC
TOXICITIES, HLH/MAS, PROLONGED CYTOPENIA and SECONDARY
HEMATOLOGICAL MALIGNANCIES
- Cytokine Release Syndrome (CRS), including fatal or
life-threatening reactions, occurred in patients following
treatment with ABECMA. Do not administer ABECMA to patients with
active infection or inflammatory disorders. Treat severe or
life-threatening CRS with tocilizumab or tocilizumab and
corticosteroids.
- Neurologic Toxicities, which may be severe or life-threatening,
occurred following treatment with ABECMA, including concurrently
with CRS, after CRS resolution, or in the absence of CRS. Monitor
for neurologic events after treatment with ABECMA. Provide
supportive care and/or corticosteroids as needed.
- Hemophagocytic Lymphohistiocytosis/Macrophage Activation
Syndrome (HLH/MAS) including fatal and life-threatening reactions,
occurred in patients following treatment with ABECMA. HLH/MAS can
occur with CRS or neurologic toxicities.
- Prolonged Cytopenia with bleeding and infection, including
fatal outcomes following stem cell transplantation for
hematopoietic recovery, occurred following treatment with
ABECMA.
- T cell malignancies have occurred following treatment of
hematologic malignancies with BCMA- and CD19-directed genetically
modified autologous T cell immunotherapies, including ABECMA
- ABECMA is available only through a restricted program under a
Risk Evaluation and Mitigation Strategy (REMS) called the ABECMA
REMS.
Warnings and Precautions:
Early Death: In KarMMa-3, a randomized (2:1), controlled
trial, a higher proportion of patients experienced death within 9
months after randomization in the ABECMA arm (45/254; 18%) compared
to the standard regimens arm (15/132; 11%). Early deaths occurred
in 8% (20/254) and 0% prior to ABECMA infusion and standard regimen
administration, respectively, and 10% (25/254) and 11% (15/132)
after ABECMA infusion and standard regimen administration,
respectively. Out of the 20 deaths that occurred prior to ABECMA
infusion, 15 occurred from disease progression, 3 occurred from
adverse events and 2 occurred from unknown causes. Out of the 25
deaths that occurred after ABECMA infusion, 10 occurred from
disease progression, 11 occurred from adverse events, and 4
occurred from unknown causes.
Cytokine Release Syndrome (CRS): CRS, including fatal or
life-threatening reactions, occurred following treatment with
ABECMA. Among patients receiving ABECMA for relapsed refractory
multiple myeloma in the KarMMa and KarMMa-3 studies (N=349), CRS
occurred in 89% (310/349), including ≥ Grade 3 CRS (Lee grading
system) in 7% (23/349) of patients and Grade 5 CRS in 0.9% (3/349)
of patients. The median time-to-onset of CRS, any grade, was 1 day
(range: 1 to 27 days), and the median duration of CRS was 5 days
(range: 1 to 63 days). In the pooled studies, the rate of ≥Grade 3
CRS was 10% (7/71) for patients treated in dose range of 460 to 510
x 106 CAR-positive T cells and 5.4% (13/241) for patients treated
in dose range of 300 to 460 x 106 CAR-positive T cells.
The most common manifestations of CRS (greater than or equal to
10%) included pyrexia (87%), hypotension (30%), tachycardia (26%),
chills (19%), hypoxia (16%). Grade 3 or higher events that may be
associated with CRS include hypotension, hypoxia,
hyperbilirubinemia, hypofibrinogenemia, ARDS, atrial fibrillation,
hepatocellular injury, metabolic acidosis, pulmonary edema,
coagulopathy, renal failure, multiple organ dysfunction syndrome
and HLH/MAS.
Identify CRS based on clinical presentation. Evaluate for and
treat other causes of fever, hypoxia, and hypotension. CRS has been
reported to be associated with findings of HLH/MAS, and the
physiology of the syndromes may overlap. HLH/MAS is a potentially
life-threatening condition. In patients with progressive symptoms
of CRS or refractory CRS despite treatment, evaluate for evidence
of HLH/MAS.
Of the 349 patients who received ABECMA in clinical trials, 226
(65%) patients received tocilizumab; 39% (135/349) received a
single dose, while 26% (91/349) received more than 1 dose of
tocilizumab. Overall, 24% (82/349) of patients received at least 1
dose of corticosteroids for treatment of CRS. Almost all patients
who received corticosteroids for CRS also received tocilizumab. For
patients treated in dose range of 460 to 510 x 106 CAR-positive T
cells, 76% (54/71) of patients received tocilizumab and 35% (25/71)
received at least 1 dose of corticosteroids for treatment of CRS.
For patients treated in dose range of 300 to 460 x 106 CAR-positive
T cells, 63% (152/241) of patients received tocilizumab and 20%
(49/241) received at least 1 dose of corticosteroid for treatment
of CRS.
Monitor patients at least daily for 7 days following ABECMA
infusion at the REMS-certified healthcare facility for signs or
symptoms of CRS and monitor patients for signs or symptoms of CRS
for at least 4 weeks after ABECMA infusion. At the first sign of
CRS, institute treatment with supportive care, tocilizumab and/or
corticosteroids as indicated. Ensure that a minimum of 2 doses of
tocilizumab are available prior to infusion of ABECMA. Counsel
patients to seek immediate medical attention should signs or
symptoms of CRS occur at any time.
Neurologic Toxicities: Neurologic toxicities, including
immune-effector cell-associated neurotoxicity (ICANS), which may be
severe or life- threatening, occurred concurrently with CRS, after
CRS resolution, or in the absence of CRS following treatment with
ABECMA.
In patients receiving ABECMA in the KarMMa and KarMMa-3 studies,
CAR T cell-associated neurotoxicity occurred in 40% (139/349),
including Grade 3 in 4% (14/349) and Grade 4 in 0.6% (2/349) of
patients. The median time to onset of neurotoxicity was 2 days
(range: 1 to 148 days). The median duration of CAR T
cell-associated neurotoxicity was 8 days (range: 1 to 720 days) in
all patients including those with ongoing neurologic events at the
time of death or data cut off. CAR T cell-associated neurotoxicity
resolved in 123 of 139 (88%) patients and median time to resolution
was 5 days (range: 1 to 245 days). One-hundred and thirty four out
of 349 (38%) patients with neurotoxicity had CRS. The onset of
neurotoxicity during CRS was observed in 93 patients, before the
onset of CRS in 12 patients, and after the CRS event in 29
patients. The rate of Grade 3 or 4 CAR T cell-associated
neurotoxicity was 5.6% (4/71) and 3.7% (9/241) for patients treated
in dose range of 460 to 510 x 106 CAR-positive T cells and 300 to
460 x 106 CAR-positive T cells, respectively. The most frequent
(greater than or equal to 5%) manifestations of CAR T
cell-associated neurotoxicity include encephalopathy (21%),
headache (15%), dizziness (8%), delirium (6%), and tremor (6%).
At the safety update for KarMMa-3 study, one patient developed
fatal neurotoxicity 43 days after ABECMA. In KarMMa, one patient
had ongoing Grade 2 neurotoxicity at the time of death. Two
patients had ongoing Grade 1 tremor at the time of data cutoff.
Cerebral edema has been associated with ABECMA in a patient in
another study in multiple myeloma. Grade 3 myelitis and Grade 3
parkinsonism have occurred after treatment with ABECMA in another
study in multiple myeloma.
Monitor patients at least daily for 7 days following ABECMA
infusion at the REMS-certified healthcare facility for signs or
symptoms of neurologic toxicities and monitor patients for signs or
symptoms of neurologic toxicities for at least 4 weeks after ABECMA
infusion and treat promptly. Rule out other causes of neurologic
symptoms. Neurologic toxicity should be managed with supportive
care and/or corticosteroids as needed. Counsel patients to seek
immediate medical attention should signs or symptoms occur at any
time.
Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage
Activation Syndrome (MAS): In patients receiving ABECMA in the
KarMMa and KarMMa-3 studies, HLH/MAS occurred in 2.9% (10/349) of
patients. All events of HLH/MAS had onset within 10 days of
receiving ABECMA, with a median onset of 6.5 days (range: 4 to 10
days) and occurred in the setting of ongoing or worsening CRS. Five
patients with HLH/MAS had overlapping neurotoxicity. The
manifestations of HLH/MAS include hypotension, hypoxia, multiple
organ dysfunction, renal dysfunction and cytopenia.
In KarMMa-3, one patient had Grade 5, two patients had Grade 4
and two patients had Grade 3 HLH/MAS. The patient with Grade 5
HLH/MAS also had Grade 5 candida sepsis and Grade 5 CRS. In another
patient who died due to stroke, the Grade 4 HLH/MAS had resolved
prior to death. Two cases of Grade 3 and one case of Grade 4
HLH/MAS had resolved.
In KarMMa, one patient treated in the 300 x 106 CAR-positive T
cells dose cohort developed fatal multi-organ HLH/MAS with CRS. In
another patient with fatal bronchopulmonary aspergillosis, HLH/MAS
was contributory to the fatal outcome. Three cases of Grade 2
HLH/MAS resolved.
HLH/MAS is a potentially life-threatening condition with a high
mortality rate if not recognized early and treated. Treatment of
HLH/MAS should be administered per institutional guidelines.
ABECMA REMS: Due to the risk of CRS and neurologic
toxicities, ABECMA is available only through a restricted program
under a Risk Evaluation and Mitigation Strategy (REMS) called the
ABECMA REMS. Further information is available at www.AbecmaREMS.com
or contact Bristol-Myers Squibb at 1-866-340-7332.
Hypersensitivity Reactions: Allergic reactions may occur
with the infusion of ABECMA. Serious hypersensitivity reactions,
including anaphylaxis, may be due to dimethyl sulfoxide (DMSO) in
ABECMA.
Infections: ABECMA should not be administered to patients
with active infections or inflammatory disorders. Severe,
life-threatening, or fatal infections occurred in patients after
ABECMA infusion.
In all patients receiving ABECMA in the KarMMa and KarMMa-3
studies, infections (all grades) occurred in 61% of patients. Grade
3 or 4 infections occurred in 21% of patients. Grade 3 or 4
infections with an unspecified pathogen occurred in 12%, viral
infections in 7%, bacterial infections in 4.3%, and fungal
infections in 1.4% of patients. Overall, 15 patients had Grade 5
infections (4.3%); 8 patients (2.3%) with infections of pathogen
unspecified, 3 patients (0.9%) with fungal infections, 3 patients
(0.9%) with viral infections, and 1 patient (0.3%) with bacterial
infection.
Monitor patients for signs and symptoms of infection before and
after ABECMA infusion and treat appropriately. Administer
prophylactic, pre-emptive, and/or therapeutic antimicrobials
according to standard institutional guidelines.
Febrile neutropenia was observed in 38% (133/349) of patients
after ABECMA infusion and may be concurrent with CRS. In the event
of febrile neutropenia, evaluate for infection and manage with
broad-spectrum antibiotics, fluids, and other supportive care as
medically indicated.
Viral Reactivation: Cytomegalovirus (CMV) infection resulting in
pneumonia and death has occurred following ABECMA administration.
Monitor and treat for CMV reactivation in accordance with clinical
guidelines. Hepatitis B virus (HBV) reactivation, in some cases
resulting in fulminant hepatitis, hepatic failure, and death, can
occur in patients treated with drugs directed against plasma cells.
Perform screening for CMV, HBV, hepatitis C virus (HCV), and human
immunodeficiency virus (HIV) in accordance with clinical guidelines
before collection of cells for manufacturing. Consider antiviral
therapy to prevent viral reactivation per local institutional
guidelines/clinical practice.
Prolonged Cytopenias: In patients receiving ABECMA in the
KarMMa and KarMMa-3 studies, 40% of patients (139/349) experienced
prolonged Grade 3 or 4 neutropenia and 42% (145/349) experienced
prolonged Grade 3 or 4 thrombocytopenia that had not resolved by
Month 1 following ABECMA infusion. In 89% (123/139) of patients who
recovered from Grade 3 or 4 neutropenia after Month 1, the median
time to recovery from ABECMA infusion was 1.9 months. In 76%
(110/145) of patients who recovered from Grade 3 or 4
thrombocytopenia, the median time to recovery was 1.9 months. Five
patients underwent stem cell therapy for hematopoietic
reconstitution due to prolonged cytopenia. The rate of Grade 3 or 4
thrombocytopenia was 62% (44/71) and 56% (135/241) for patients
treated in dose range of 460 to 510 x 106 CAR-positive T cells and
300 to 460 x 106 CAR-positive T cells, respectively.
Monitor blood counts prior to and after ABECMA infusion. Manage
cytopenia with myeloid growth factor and blood product transfusion
support according to local institutional guidelines.
Hypogammaglobulinemia: In all patients receiving ABECMA
in the KarMMa and KarMMa-3 studies, hypogammaglobulinemia was
reported as an adverse event in 13% (46/349) of patients;
laboratory IgG levels fell below 500 mg/dL after infusion in 37%
(130/349) of patients treated with ABECMA.
Hypogammaglobulinemia either as an adverse reaction or
laboratory IgG level below 500 mg/dL after infusion occurred in 45%
(158/349) of patients treated with ABECMA. Forty-one percent of
patients received intravenous immunoglobulin (IVIG) post-ABECMA for
serum IgG <400 mg/dL.
Monitor immunoglobulin levels after treatment with ABECMA and
administer IVIG for IgG <400 mg/dl. Manage appropriately per
local institutional guidelines, including infection precautions and
antibiotic or antiviral prophylaxis.
Use of Live Vaccines: The safety of immunization with live viral
vaccines during or after ABECMA treatment has not been studied.
Vaccination with live virus vaccines is not recommended for at
least 6 weeks prior to the start of lymphodepleting chemotherapy,
during ABECMA treatment, and until immune recovery following
treatment with ABECMA.
Secondary Malignancies: Patients treated with ABECMA may
develop secondary malignancies. In KarMMa-3, myeloid neoplasms
(four cases of myelodysplastic syndrome and one case of acute
myeloid leukemia) occurred in 2.2% (5/222) of patients following
treatment with ABECMA compared to none in the standard regimens arm
at the time of the safety update. The median time to onset of
myeloid neoplasm from ide-cel infusion was 338 days (Range: 277 to
794 days). Three of these five patients have died following the
development of myeloid neoplasm. One out of the five cases of
myeloid neoplasm occurred after initiation of subsequent
antimyeloma therapy.
T cell malignancies have occurred following treatment of
hematologic malignancies with BCMA- and CD19-directed genetically
modified autologous T cell immunotherapies, including ABECMA.
Mature T cell malignancies, including CAR-positive tumors, may
present as soon as weeks following infusion, and may include fatal
outcomes.
Monitor life-long for secondary malignancies. In the event that
a secondary malignancy occurs, contact Bristol-Myers Squibb at
1‑888‑805‑4555 for reporting and to obtain instructions on
collection of patient samples for testing of secondary
malignancy.
Effects on Ability to Drive and Operate Machinery: Due to
the potential for neurologic events, including altered mental
status or seizures, patients receiving ABECMA are at risk for
altered or decreased consciousness or coordination in the 8 weeks
following ABECMA infusion. Advise patients to refrain from driving
and engaging in hazardous occupations or activities, such as
operating heavy or potentially dangerous machinery, during this
initial period.
Adverse Reactions: The most common nonlaboratory adverse
reactions (incidence greater than or equal to 20%) include pyrexia,
CRS, hypogammaglobulinemia, infections – pathogen unspecified,
musculoskeletal pain, fatigue, febrile neutropenia, hypotension,
tachycardia, diarrhea, nausea, headache, chills, upper respiratory
tract infection, encephalopathy, edema, dyspnea and viral
infections.
Please see full Prescribing Information, including Boxed
WARNINGS and Medication Guide.
Bristol Myers Squibb: Creating a Better
Future for People with Cancer
Bristol Myers Squibb is inspired by a single vision —
transforming patients’ lives through science. The goal of the
company’s cancer research is to deliver medicines that offer each
patient a better, healthier life and to make cure a possibility.
Building on a legacy across a broad range of cancers that have
changed survival expectations for many, Bristol Myers Squibb
researchers are exploring new frontiers in personalized medicine
and, through innovative digital platforms, are turning data into
insights that sharpen their focus. Deep understanding of causal
human biology, cutting-edge capabilities and differentiated
research platforms uniquely position the company to approach cancer
from every angle.
Cancer can have a relentless grasp on many parts of a patient’s
life, and Bristol Myers Squibb is committed to taking actions to
address all aspects of care, from diagnosis to survivorship. As a
leader in cancer care, Bristol Myers Squibb is working to empower
all people with cancer to have a better future.
Learn more about the science behind cell therapy and ongoing
research at Bristol Myers Squibb here.
About Bristol Myers
Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose
mission is to discover, develop and deliver innovative medicines
that help patients prevail over serious diseases. For more
information about Bristol Myers Squibb, visit us at BMS.com or
follow us on LinkedIn, Twitter, YouTube, Facebook and
Instagram.
About 2seventy bio
Our name, 2seventy bio, reflects why we do what we do - TIME.
Cancer rips time away, and our goal is to work at the maximum speed
of translating human thought into action – 270 miles per hour – to
give the people we serve more time. We are building the leading
immuno-oncology cell therapy company, focused on discovering and
developing new therapies that truly disrupt the cancer treatment
landscape. With a deep understanding of the human body’s immune
response to tumor cells and how to translate cell therapies into
practice, we’re applying this knowledge to deliver next generation
cellular therapies that focus on a broad range of hematologic
malignancies, including the first FDA-approved CAR T cell therapy
for multiple myeloma, as well as solid tumors. Our research and
development are focused on delivering therapies that are designed
with the goal to “think” smarter and faster than the disease.
Importantly, we remain focused on accomplishing these goals by
staying genuine and authentic to our “why” and keeping our people
and culture top of mind every day.
For more information, visit www.2seventybio.com.
Follow 2seventy bio on social media: Twitter and LinkedIn.
2seventy bio is a trademark of 2seventy bio, Inc.
Bristol Myers Squibb Cautionary
Statement Regarding Forward-Looking Statements
This press release contains “forward-looking statements” within
the meaning of the Private Securities Litigation Reform Act of 1995
regarding, among other things, the research, development and
commercialization of pharmaceutical products. All statements that
are not statements of historical facts are, or may be deemed to be,
forward-looking statements. Such forward-looking statements are
based on current expectations and projections about our future
financial results, goals, plans and objectives and involve inherent
risks, assumptions and uncertainties, including internal or
external factors that could delay, divert or change any of them in
the next several years, that are difficult to predict, may be
beyond our control and could cause our future financial results,
goals, plans and objectives to differ materially from those
expressed in, or implied by, the statements. These risks,
assumptions, uncertainties and other factors include, among others,
whether Abecma® (idecabtagene vicleucel) for the indication
described in this release will be commercially successful, any
marketing approvals, if granted, may have significant limitations
on their use, and that continued approval of Abecma for such
indication described in this release may be contingent upon
verification and description of clinical benefit in confirmatory
trials. No forward-looking statement can be guaranteed.
Forward-looking statements in this press release should be
evaluated together with the many risks and uncertainties that
affect Bristol Myers Squibb’s business and market, particularly
those identified in the cautionary statement and risk factors
discussion in Bristol Myers Squibb’s Annual Report on Form 10-K for
the year ended December 31, 2023, as updated by our subsequent
Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and
other filings with the Securities and Exchange Commission. The
forward-looking statements included in this document are made only
as of the date of this document and except as otherwise required by
applicable law, Bristol Myers Squibb undertakes no obligation to
publicly update or revise any forward-looking statement, whether as
a result of new information, future events, changed circumstances
or otherwise.
2seventy bio Cautionary Note Regarding
Forward-Looking Statements
This press release contains “forward-looking statements” within
the meaning of the Private Securities Litigation Reform Act of 1995
regarding, among other things, the research, development and
commercialization of Abecma® (idecabtagene vicleucel). All
statements that are not statements of historical facts are, or may
be deemed to be, forward-looking statements. Such forward-looking
statements are based on historical performance and current
expectations and projections about our future financial results,
goals, plans and objectives and involve inherent risks, assumptions
and uncertainties, including internal or external factors that
could delay, divert or change any of them in the next several
years, that are difficult to predict, may be beyond our control and
could cause our future financial results, goals, plans and
objectives to differ materially from those expressed in, or implied
by, the statements. These risks, assumptions, uncertainties and
other factors include, among others, the possibility that Abecma
may not receive FDA approval for the indication described in this
release in the currently anticipated timeline or at all, that any
marketing approvals, if granted, may have significant limitations
on their use, that Abecma may not be commercially successful and
that collaboration with Bristol Myers Squibb may not continue or be
successful. No forward-looking statement can be guaranteed.
Forward-looking statements in this press release should be
evaluated together with the many risks and uncertainties that
affect 2seventy bio’s business, particularly those identified in
the risk factors discussion in 2seventy bio’s Annual Report on Form
10-K, as updated by our subsequent Quarterly Reports on Form 10-Q,
Current Reports on Form 8-K and other filings with the Securities
and Exchange Commission. The forward-looking statements included in
this document are made only as of the date of this document and
except as otherwise required by applicable law, 2seventy bio
undertakes no obligation to publicly update or revise any
forward-looking statement, whether as a result of new information,
future events, changed circumstances or otherwise.
Hyperlinks are provided as a convenience and for informational
purposes only. Neither Bristol Myers Squibb nor 2seventy bio bears
responsibility for the security or content of external websites or
websites outside of their respective control.
corporatefinancial-news
View source
version on businesswire.com: https://www.businesswire.com/news/home/20240403030392/en/
Bristol Myers Squibb
Media Inquiries: media@bms.com
Investors: investor.relations@bms.com
2seventy bio
Investors:
Elizabeth Pingpank 860-463-0469
elizabeth.pingpank@2seventybio.com
Media:
Jenn Snyder 617-448-0281 jenn.snyder@2seventybio.com
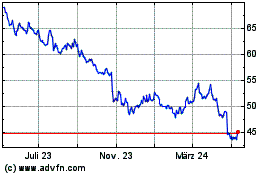
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
Von Jan 2025 bis Feb 2025
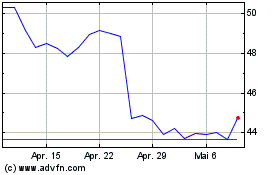
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
Von Feb 2024 bis Feb 2025