Bristol Myers Squibb (NYSE: BMY) today announced the
presentation of data across its oncology and hematology portfolio
at the upcoming 2024 American Society of Clinical Oncology (ASCO)
Annual Meeting and the European Hematology Association (EHA) 2024
Hybrid Congress. Data from more than 130 company-sponsored studies,
investigator-sponsored studies, and collaborations showcase results
spanning approximately 25 cancer types and serious blood
disorders.
“At this year’s ASCO and EHA meetings, we have the opportunity
to share data across our robust and differentiated oncology
portfolio including new data from pivotal studies, data that
reinforce the longer-term impact our medicines are having for
patients, and emerging science in the oncology space,” said Samit
Hirawat, M.D., executive vice president, chief medical officer,
Drug Development, Bristol Myers Squibb. “We are focused on
advancing critical research across immuno-oncology, targeted
therapy, protein degradation, cell therapy, and radiopharmaceutical
therapy, all with the goal of delivering potentially transformative
treatment options that help provide long-term benefit for
patients.”
Key data being presented by Bristol Myers Squibb at ASCO and EHA
include:
New pivotal data
- Progression-free survival and overall response rate data from
the Phase 3 KRYSTAL-12 study evaluating KRAZATI® (adagrasib) as a
monotherapy in patients with pretreated locally advanced or
metastatic non-small cell lung cancer (NSCLC) harboring a KRASG12C
mutation. (ASCO)
- First disclosure of results from the Phase 3 CheckMate -9DW
trial demonstrating overall survival benefit with Opdivo®
(nivolumab) plus Yervoy® (ipilimumab) vs. investigator’s choice of
lenvatinib or sorafenib as a first-line treatment for patients with
advanced hepatocellular carcinoma (HCC). (ASCO)
Data strengthening the profile of our existing
portfolio
- Three-year follow-up data from the Phase 3 RELATIVITY-047 study
demonstrating sustained responses with Opdualag™ (nivolumab and
relatlimab-rmbw) in previously untreated metastatic or unresectable
melanoma. (ASCO)
- Five-year data from the Phase 3 CheckMate -9LA trial showing
favorable clinical outcomes and durable survival benefit in
patients with metastatic NSCLC treated with Opdivo plus Yervoy with
chemotherapy vs. chemotherapy. (ASCO)
- Four-year follow-up data from the Phase 3 CheckMate -816 trial
reinforcing neoadjuvant Opdivo plus chemotherapy as a treatment in
resectable NSCLC. (ASCO)
- Exploratory analysis from the Phase 3 CheckMate -77T trial
supporting the potential use of a perioperative Opdivo-based
regimen as a treatment option for patients with resectable NSCLC,
regardless of nodal status. (ASCO)
- Multiple subgroup analyses from the Phase 1/2 TRANSCEND CLL
004, Phase 1 TRANSCEND NHL 001 (MCL cohort) and Phase 2 TRANSCEND
FL studies reinforcing the deep and durable responses with
Breyanzi® (lisocabtagene maraleucel), demonstrating consistent
clinical outcomes in relapsed/refractory chronic lymphocytic
leukemia (CLL), relapsed/refractory mantle cell lymphoma (MCL) and
relapsed/refractory follicular lymphoma (FL) across a broad study
population. (ASCO/EHA)
Emerging science
- Efficacy and safety data from the Phase 2/3 RELATIVITY-048
trial evaluating the triplet combination of nivolumab, relatlimab,
and ipilimumab in patients with advanced melanoma. (ASCO)
- Safety and efficacy data from the Phase 1b portion of the
ACTION-1 trial of RYZ101 (an alpha-emitting radiopharmaceutical in
development for SSTR2+ solid tumors) in gastroenteropancreatic
neuroendocrine tumors (GEP-NET) progressing after 177Lu
somatostatin analogue (SSA) therapy. (ASCO)
- First results from the Phase 1 study of GPRC5D-directed CAR T
cell therapy (BMS-986393/CC-95266) showcasing promising preliminary
efficacy and safety outcomes with a single infusion of BMS-986393
in patients with relapsed or refractory multiple myeloma, including
in patients with prior BCMA-directed therapy, who have received one
to three prior regimens. (EHA)
- New Phase 1/2 data from the targeted protein degradation
platform including the novel oral CELMoD agents iberdomide in newly
diagnosed multiple myeloma, mezigdomide in relapsed/refractory
multiple myeloma, and golcadomide in first-line LBCL and
relapsed/refractory FL, reinforcing promising activity.
(ASCO/EHA)
Please see below for Important Safety Information and full
Prescribing Information for Opdualag, Opdivo, Opdivo + Yervoy,
Augtyro™ (repotrectinib), Reblozyl® (luspatercept-aamt) and
KRAZATI.
Please see below for Important Safety Information and full
Prescribing Information, including Boxed Warnings, for Abecma®
(idecabtagene vicleucel), Breyanzi and Inrebic® (fedratinib).
Reblozyl is being developed and commercialized through a global
collaboration with Merck following Merck’s acquisition of Acceleron
Pharma, Inc. in November 2021.
Summary of
Presentations:
Select Bristol Myers Squibb studies at the 2024 ASCO Annual
Meeting include:
(all times in Central Time)
Abstract Title
Author
Presentation
Type/#
Session Title
Session
Date/Time
(CDT)
Acute Myeloid Leukemia (AML)
A post-hoc analysis of outcomes of
patients with acute myeloid leukemia with myelodysplasia-related
changes (AML-MRC) who received oral azacitidine (Oral-AZA)
maintenance therapy in the QUAZAR AML-001 study.
Stéphane De Botton
Poster
Abstract #6522
Hematologic Malignancies— Leukemia,
Myelodysplastic Syndromes, and Allotransplant
Monday,
June 3, 2024
9:00 AM - 12:00 PM
Bladder Cancer
SOGUG-Vexillum: Phase II non-randomized
clinical trial of nivolumab/ipilimumab maintenance following
first-line chemotherapy in unresectable locally advanced or
metastatic urothelial cancer.
Guillermo De Velasco
Poster
Abstract #4576
Genitourinary Cancer—Kidney and
Bladder
Sunday,
June 2, 2024
9:00 AM - 12:00 PM
Characterization of complete responders to
nivolumab + gemcitabine-cisplatin vs gemcitabine-cisplatin alone
and patients with lymph node-only metastatic urothelial carcinoma
from the CheckMate 901 trial.
Matthew D. Galsky
Oral
Abstract #4509
Genitourinary Cancer—Kidney and
Bladder
Monday,
June 3, 2024
8:00 AM - 11:00 AM
Breast Cancer
Phase 2 study of novel HER2-targeting,
TLR7/8 immune-stimulating antibody conjugate (ISAC) BDC-1001
(trastuzumab imbotolimod) +/- pertuzumab (P) in patients (pts) with
HER2-positive metastatic breast cancer (MBC) previously treated
with trastuzumab deruxtecan (T-DXd).
Mark Pegram
Poster
Abstract #TPS1121
Breast Cancer—Metastatic
Sunday,
June 2, 2024
9:00 AM - 12:00 PM
Chronic Lymphocytic Leukemia
(CLL)
Evaluating CR as a surrogate endpoint for
PFS in R/R chronic lymphocytic leukemia/small lymphocytic lymphoma
(CLL/SLL): A meta-analysis of randomized controlled trials
(RCT).
Lin Wang
Poster
Abstract #7046
Hematologic Malignancies—Lymphoma and
Chronic Lymphocytic Leukemia
Monday,
June 3, 2024
9:00 AM - 12:00 PM
Association between treatment (tx)
response and PFS and OS in R/R chronic lymphocytic leukemia (CLL)
or small lymphocytic lymphoma (SLL): A 12-month landmark (LM)
meta-analysis.
Xin Wang
Poster
Abstract #7047
Hematologic Malignancies—Lymphoma and
Chronic Lymphocytic Leukemia
Monday,
June 3, 2024
9:00 AM - 12:00 PM
Colorectal Cancer (CRC)
A phase 2 study evaluating response and
biomarkers in patients with microsatellite stable (MSS) advanced
colorectal cancer (CRC) treated with nivolumab/relatlimab.
Eric Christenson
Poster
Abstract #3554
Gastrointestinal Cancer—Colorectal and
Anal
Saturday,
June 1, 2024
1:30 PM - 4:30 PM
Nivolumab (NIVO) plus ipilimumab (IPI) vs
chemotherapy (chemo) as first-line (1L) treatment for
microsatellite instability-high/mismatch repair-deficient
(MSI-H/dMMR) metastatic colorectal cancer (mCRC): Expanded efficacy
analysis from CheckMate 8HW.
Heinz-Joseph Lenz
Oral
Abstract #3503
Gastrointestinal Cancer—Colorectal and
Anal
Sunday,
June 2, 2024
8:00 AM - 11:00 AM
Esophageal Cancer (EC) and
Gastrointestinal Cancers
Nivolumab (NIVO) plus chemotherapy (chemo)
or ipilimumab (IPI) vs chemo as first-line (1L) treatment for
advanced esophageal squamous cell carcinoma (ESCC): 45-month (mo)
follow-up from CheckMate 648.
Ian Chau
Poster
Abstract #4034
Gastrointestinal Cancer—Gastroesophageal,
Pancreatic, and Hepatobiliary
Saturday,
June 1, 2024
1:30 PM - 4:30 PM
Nivolumab (NIVO) + chemotherapy (chemo) vs
chemo as first-line (1L) treatment for advanced gastric
cancer/gastroesophageal junction cancer/esophageal adenocarcinoma
(GC/GEJC/EAC): 4-year follow-up of CheckMate 649.
Elena Elimova
Poster
Abstract #4040
Gastrointestinal Cancer—Gastroesophageal,
Pancreatic, and Hepatobiliary
Saturday,
June 1, 2024
1:30 PM - 4:30 PM
Updated quality-adjusted time without
symptoms or toxicity (Q-TWiST) analysis of nivolumab plus
chemotherapy versus chemotherapy alone as first-line (1L) treatment
for advanced gastric cancer, gastroesophageal junction cancer, or
esophageal adenocarcinoma (GC/GEJC/EAC): 4-year (yr) follow-up from
CheckMate 649 (CM 649).
Daniel Lin
Poster
Abstract #4044
Gastrointestinal Cancer—Gastroesophageal,
Pancreatic, and Hepatobiliary
Saturday,
June 1, 2024
1:30 PM - 4:30 PM
A phase II/III study of peri-operative
nivolumab (nivo) and ipilimumab (ipi) in patients (pts) with
locoregional esophageal (E) and gastroesophageal junction (GEJ)
adenocarcinoma: Results of the neoadjuvant pathologic complete
response (pCR) rate (ECOG-ACRIN EA2174).
Jennifer Rachel Eads
Oral
Abstract #4000
Gastrointestinal Cancer—Gastroesophageal,
Pancreatic, and Hepatobiliary
Tuesday,
June 4, 2024
9:45 AM - 12:45 PM
Hepatocellular Carcinoma (HCC)
Nivolumab (NIVO) plus ipilimumab (IPI) vs
lenvatinib (LEN) or sorafenib (SOR) as first-line treatment for
unresectable hepatocellular carcinoma (uHCC): First results from
CheckMate 9DW.
Peter Robert Galle
Oral
Abstract #LBA4008
Gastrointestinal Cancer—Gastroesophageal,
Pancreatic, and Hepatobiliary
Tuesday,
June 4, 2024
9:45 AM - 12:45 PM
Melanoma
Efficacy and safety of triplet nivolumab,
relatlimab, and ipilimumab (NIVO + RELA + IPI) in advanced
melanoma: Results from RELATIVITY-048.
Paolo Antonio Ascierto
Oral
Abstract #9504
Melanoma/Skin Cancers
Friday,
May 31, 2024
2:45 PM - 5:45 PM
Nivolumab (NIVO) plus relatlimab (RELA) vs
NIVO in previously untreated metastatic or unresectable melanoma
(RELATIVITY-047): Overall survival (OS) and melanoma-specific
survival (MSS) outcomes at 3 years.
Hussein A. Tawbi
Poster
Abstract #9524
Melanoma/Skin Cancers
Saturday,
June 1, 2024
1:30 PM - 4:30 PM
Efficacy and safety of first-line (1L)
nivolumab plus relatlimab (NIVO + RELA) versus NIVO plus ipilimumab
(NIVO + IPI) in advanced melanoma: An updated indirect treatment
comparison (ITC).
Dirk Schadendorf
Poster
Abstract #9557
Melanoma/Skin Cancers
Saturday,
June 1, 2024
1:30 PM - 4:30 PM
First-line treatment preferences for
advanced melanoma among oncologists and patients in the US: A
discrete choice experiment.
Michael A. Postow
Poster
Abstract #9539
Melanoma/Skin Cancers
Saturday,
June 1, 2024
1:30 PM - 4:30 PM
A phase 2, open-label, 2-cohort study to
evaluate patient preference for nivolumab (NIVO) + relatlimab
(RELA) fixed-dose combination (FDC) subcutaneous (SC) vs NIVO +
RELA FDC intravenous (IV) and NIVO SC vs NIVO IV in participants
with melanoma.
Steven Y. Liu
Poster
Abstract #TPS9619
Melanoma/Skin Cancers
Saturday,
June 1, 2024
1:30 PM - 4:30 PM
Multiple Myeloma (MM)
Association of patient (pt) factors and
pharmacodynamic biomarkers with progression-free survival (PFS)
after idecabtagene vicleucel (ide-cel) in pts from KarMMa-3.
Bertrand Arnulf
Poster
Abstract #7527
Hematologic Malignancies—Plasma Cell
Dyscrasia
Monday,
June 3, 2024
9:00 AM - 12:00 PM
Impact of renal impairment (RI) on
pharmacokinetics (PK) and clinical outcomes with mezigdomide plus
dexamethasone (DEX) in relapsed/refractory multiple myeloma
(RRMM).
Suzanne Trudel
Poster
Abstract #7539
Hematologic Malignancies—Plasma Cell
Dyscrasia
Monday,
June 3, 2024
9:00 AM - 12:00 PM
Validation of prototype biomarkers to
identify risk factors of inflammatory adverse events (iAEs)
following idecabtagene vicleucel (ide-cel) infusion in patients
with relapsed and refractory multiple myeloma (RRMM) in
KarMMa-3.
Clara Amorosi
Poster
Abstract #7529
Hematologic Malignancies—Plasma Cell
Dyscrasia
Monday,
June 3, 2024
9:00 AM - 12:00 PM
Myelodysplastic Syndromes (MDS)
Preliminary safety and efficacy of oral
azacitidine (Oral-AZA) in patients (pts) with low-/Intermediate
(Int)-risk myelodysplastic syndromes (MDS): Phase 2 results from
the ASTREON trial.
Guillermo Garcia-Manero
Rapid Oral
Abstract #6509
Hematologic Malignancies—Leukemia,
Myelodysplastic Syndromes, and Allotransplant
Saturday,
June 1, 2024
8:00 AM - 9:30 AM
Clinical benefit of luspatercept treatment
(tx) in transfusion-dependent (TD), erythropoiesis-stimulating
agent (ESA)-naive patients (pts) with very low-, low- or
intermediate-risk myelodysplastic syndromes (MDS) in the COMMANDS
trial.
Amer Methqal Zeidan
Poster
Abstract #6565
Hematologic Malignancies—Leukemia,
Myelodysplastic Syndromes, and Allotransplant
Monday,
June 3, 2024
9:00 AM - 12:00 PM
Non-Hodgkin Lymphoma (includes DLBCL,
LBCL, FL, MCL, etc.)
Lisocabtagene maraleucel (liso-cel) in
patients (pt) with R/R mantle cell lymphoma (MCL): Subgroup
analyses by number of prior systemic lines of therapy (LOT) and by
response to prior Bruton tyrosine kinase inhibitor (BTKi) from the
TRANSCEND NHL 001 MCL cohort (TRANSCEND-MCL).
M. Lia Palomba
Rapid Oral
Abstract
#7016
Hematologic Malignancies—Lymphoma and
Chronic Lymphocytic Leukemia
Sunday,
June 2, 2024
4:30 PM - 6:00 PM
Lisocabtagene maraleucel (liso-cel) vs
standard of care (SOC) with salvage chemotherapy (CT) followed by
autologous stem cell transplantation (ASCT) as second-line (2L)
treatment in patients (pt) with R/R large B-cell lymphoma (LBCL):
3-year follow-up (FU) from the randomized, phase 3 TRANSFORM
study.
Manali Kirtikumar Kamdar
Rapid Oral
Abstract #7013
Hematologic Malignancies—Lymphoma and
Chronic Lymphocytic Leukemia
Sunday,
June 2, 2024
4:30 PM - 6:00 PM
Real-world outcomes of lisocabtagene
maraleucel (liso-cel) in patients (pt) with Richter transformation
(RT) from the Center for International Blood and Marrow Transplant
Research (CIBMTR).
Allison Marie Winter
Rapid Oral
Abstract #7010
Hematologic Malignancies—Lymphoma and
Chronic Lymphocytic Leukemia
Sunday,
June 2, 2024
4:30 PM - 6:00 PM
Impact of clinical response and AEs on
health-related quality of life (HRQoL) in patients (pts) with R/R
large B-cell lymphoma (LBCL): Pooled data from 4 lisocabtagene
maraleucel (liso-cel) trials.
Patrick Connor Johnson
Poster
Abstract #11105
Quality Care/Health Services Research
Monday,
June 3, 2024
9:00 AM - 12:00 PM
Estimating the health care costs
associated with receipt of lisocabtagene maraleucel: Insights from
adults with mantle cell lymphoma (TRANSCEND NHL 001).
Tycel Jovelle Phillips
Poster
Abstract #7028
Hematologic Malignancies—Lymphoma and
Chronic Lymphocytic Leukemia
Monday,
June 3, 2024
9:00 AM - 12:00 PM
Impact of bridging therapy (BT) on
lisocabtagene maraleucel (liso-cel) treatment in patients (pt) with
R/R follicular lymphoma (FL).
M. Lia Palomba
Poster
Abstract #7068
Hematologic Malignancies—Lymphoma and
Chronic Lymphocytic Leukemia
Monday,
June 3, 2024
9:00 AM - 12:00 PM
Patients (pts) with R/R large B-cell
lymphoma (LBCL) treated with lisocabtagene maraleucel (liso-cel)
nonconforming product (NCP) under the Expanded Access Protocol
(EAP).
Mecide Meric Gharibo
Poster
Abstract #7026
Hematologic Malignancies—
Lymphoma and Chronic Lymphocytic
Leukemia
Monday,
June 3, 2024
9:00 AM - 12:00 PM
Non-Small Cell Lung Cancer
(NSCLC)
KRYSTAL-12: Phase 3 Study of Adagrasib
versus Docetaxel in Patients with Previously Treated
Advanced/Metastatic Non-Small Cell Lung Cancer (NSCLC) Harboring a
KRASG12C Mutation.
Tony Mok
Oral
Abstract #LBA8509
Clinical Science Symposium—Targeting KRAS
in Non-Small Cell Lung Cancer
Saturday,
June 1, 2024
1:15 PM - 2:45 PM
Neoadjuvant nivolumab (NIVO) +
chemotherapy (chemo) vs chemo in patients (pts) with resectable
NSCLC: 4-year update from CheckMate 816.
Jonathan Spicer
Rapid Oral
Abstract #LBA8010
Lung Cancer—Non-Small Cell
Local-Regional/Small Cell/Other Thoracic Cancers
Sunday,
June 2, 2024
4:30 PM - 6:00 PM
Clinical outcomes with perioperative
nivolumab (NIVO) by nodal status among patients (pts) with stage
III resectable NSCLC: Results from the phase 3 CheckMate 77T
study.
Tina Cascone
Oral
Abstract #LBA8007
Lung Cancer—Non-Small Cell
Local-Regional/Small Cell/Other Thoracic Cancers
Monday,
June 3, 2024
8:00 AM - 11:00 AM
Correlation of the combination of
CT-derived tumor texture and vessel tortuosity on survival outcomes
for immunotherapy but not for chemotherapy in metastatic non-small
cell lung cancer (mNSCLC): Results from a CheckMate227 (CM227)
subset.
Pushkar Mutha
Poster
Abstract #8610
Lung cancer—Non-Small Cell Metastatic
Monday,
June 3, 2024
1:30 PM - 4:30 PM
Five-year outcomes with first-line (1L)
nivolumab + ipilimumab + chemotherapy (N + I + C) vs C in patients
(pts) with metastatic NSCLC (mNSCLC) in CheckMate 9LA.
Martin Reck
Poster
Abstract #8560
Lung cancer—Non-Small Cell Metastatic
Monday,
June 3, 2024
1:30 PM - 4:30 PM
Repotrectinib in tyrosine kinase inhibitor
(TKI)-naïve patients (pts) with advanced ROS1 fusion-positive
(ROS1+) NSCLC in the phase 1/2 TRIDENT-1 trial: Clinical update,
treatment beyond progression and subsequent therapies.
Alexander Drilon
Poster
Abstract #8522
Lung cancer—Non-Small Cell Metastatic
Monday,
June 3, 2024
1:30 PM - 4:30 PM
Pancreatic Cancer
Phase Ib portion of the ACTION-1 phase
Ib/3 trial of RYZ101 in gastroenteropancreatic neuroendocrine
tumors (GEP-NET) progressing after 177Lu somatostatin analogue
(SSA) therapy: Safety and efficacy findings.
Daniel Halperin
Poster
Abstract #3091
Developmental Therapeutics—Molecularly
Targeted Agents and Tumor Biology
Saturday,
June 1, 2024
9:00 AM - 12:00 PM
Renal Cell Carcinoma (RCC)
Health-related quality of life (HRQoL)
with nivolumab (NIVO) subcutaneous (SC) or intravenous (IV) in
patients (pts) with advanced or metastatic clear cell renal cell
carcinoma (ccRCC) who have received prior therapy in the phase 3
CheckMate 67T trial.
Saby George
Poster
Abstract #4535
Genitourinary Cancer—Kidney and
Bladder
Sunday,
June 2, 2024
9:00 AM - 12:00 PM
Subcutaneous (SC) nivolumab (NIVO) vs
intravenous (IV) NIVO in patients with previously treated advanced
or metastatic clear cell renal cell carcinoma (ccRCC): Safety and
patient-reported outcomes (PROs) of the randomized phase 3
CheckMate 67T trial.
Maria T. Bourlon
Poster
Abstract #4532
Genitourinary Cancer—Kidney and
Bladder
Sunday,
June 2, 2024
9:00 AM - 12:00 PM
Intratumoral T-cell infiltration and
response to nivolumab plus ipilimumab in patients with metastatic
clear cell renal cell carcinoma from the CheckMate-214 trial.
Sayed Matar
Poster
Abstract #4536
Genitourinary Cancer— Kidney and
Bladder
Sunday,
June 2, 2024
9:00 AM - 12:00 PM
Partitioned overall survival:
Comprehensive analysis of survival states over 4 years in CheckMate
9ER comparing first-line nivolumab plus cabozantinib versus
sunitinib in advanced renal cell carcinoma (aRCC).
Charlene Mantia
Oral
Abstract #4507
Genitourinary Cancer—Kidney and
Bladder
Monday,
June 3, 2024
8:00 AM - 11:00 AM
Brain Cancer
Phase II study of enasidenib in
IDH2-mutated malignant sinonasal and skull base tumors.
Elisabetta Xue
Poster
#TPS3183
Developmental Therapeutics—Molecularly
Targeted Agents and Tumor Biology
Saturday,
June 1, 2024
9:00 AM - 12:00 PM
All abstracts, except late-breaking abstracts, are available on
the ASCO website as of 5:00 PM EDT on Thursday, May 23. All
late-breaking abstracts will be available on the ASCO website at
8:00 AM EDT on the day of the scientific session for the abstract
presentation.
Select Bristol Myers Squibb studies at the 2024 EHA Congress
include:
(all times in Eastern Daylight and Central European
Time)
Abstract Title
Author
Presentation
Type
Session Date/Time
(EDT/CET)
Acute Myeloid Leukemia (AML)
A post hoc analysis of outcomes of
patients with acute myeloid leukemia with myelodysplasia-related
changes who received oral azacitidine maintenance therapy in the
QUAZAR AML-001 study.
Maria Teresa Voso
Oral
Abstract #S141
Saturday, June 15, 2024
11:30 AM - 12:45 PM (16:30 - 17:45
CET)
Impact of TP53 mutations in patients with
acute myeloid leukemia (AML) during oral azacitidine maintenance
therapy: Outcomes from the QUAZAR AML-001 trial.
Andrew H. Wei
Poster
Abstract #P560
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Chronic Lymphocytic Leukemia
(CLL)
Characteristics associated with response
to lisocabtagene maraleucel (liso-cel) in patients (PTS) with R/R
CLL/SLL: Exploratory analyses from TRANSCEND CLL 004.
William G. Wierda
Oral
Abstract #S158
Sunday, June 16, 2024
6:30 AM - 7:45 AM (11:30 - 12:45 CET)
Multiple Myeloma (MM)
Disease characteristics and survival
outcomes in patients with relapsed and refractory multiple myeloma
by extramedullary disease status: findings from the Connect® MM
disease registry.
Hans Lee
Poster
Abstract #P930
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Safety and preliminary efficacy of
BMS-986393, a GPRC5D CAR T cell therapy, in patients with
relapsed/refractory (RR) multiple myeloma (MM) and 1-3 prior
regimens: First results from a phase 1 study.
Omar Nadeem
Poster
Abstract #P951
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Idecabtagene vicleucel (ide-cel) in
patients (pts) with clinical high-risk early relapse multiple
myeloma (MM) without front-line (1L) autologous stem cell
transplantation (ASCT): KarMMa-2 cohort 2b.
Xavier Leleu
Oral
Abstract #S208
Saturday, June 15, 2024
11:30 PM - 12:45 PM (16:30 - 17:45
CET)
Association of patient factors and
pharmacodynamic biomarkers with progression-free survival after
idecabtagene vicleucel in patients from KarMMa-3.
Bertrand Arnulf
Poster Abstract #P876
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Iberdomide is immune stimulatory and
induces deep anti-myeloma activity across doses in combination with
daratumumab in patients with TNE NDMM from the CC-220-MM-001
study.
Michael Amatangelo
Poster
Abstract #P847
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Mezigdomide (mezi), tazemetostat (taz),
and dexamethasone (dex) in patients (PTS) with relapsed/refractory
multiple myeloma (RRMM): Preliminary results from the CA057-003
trial.
Luciano Costa
Poster
Abstract #P903
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Improved disease status pre-infusion leads
to better outcomes with standard of care idecabtagene vicleucel
(ide-cel) in patients with relapsed refractory multiple myeloma
(RRMM).
Aimaz Afrough
Poster
Abstract #P939
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Myelodysplastic Syndromes (MDS)
Real-world dose escalation and outcomes
among patients with lower-risk myelodysplastic syndromes receiving
luspatercept in clinical practice.
Kashyap Patel
Poster
Abstract #P768
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Quantifying the relationship between
transfusion independence and overall survival in lower-risk
myelodysplastic syndromes.
Luca Malcovati
Poster
Abstract #P782
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Value of early luspatercept use in
lower-risk myelodysplastic syndromes (LR-MDS).
David Valcárcel
Poster
Abstract #P789
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Relationship between haemoglobin and
quality of life in transfusion-dependent patients with lower-risk
myelodysplastic syndrome receiving luspatercept or epoetin
alfa.
Esther Oliva
Poster
Abstract #P774
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Luspatercept improves hematopoiesis in
lower-risk myelodysplastic syndromes (MDS): Comparative biomarker
analysis of ring sideroblast-positive and -negative subgroups from
the phase 3 COMMANDS study.
Sheida Hayati
Poster
Abstract #P763
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Clinical benefit of luspatercept in
transfusion-dependent, erythropoiesis-stimulating agent-naive
patients with very low-, low- or intermediate-risk myelodysplastic
syndromes in the COMMANDS trial.
Valeria Santini
Poster
Abstract #P785
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Multilineage and safety results from the
COMMANDS trial in transfusion-dependent, erythropoiesis-stimulating
agent-naive patients with very low-, low- or intermediate-risk
myelodysplastic syndromes.
Guillermo Garcia-Manero
Poster
Abstract #P780
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Comparative analysis of clinical benefit
by genomic landscape and mutational burden of luspatercept versus
epoetin alfa in lower-risk myelodysplastic syndromes (MDS) in the
Phase 3 COMMANDS study.
Rami S Komrokji
Poster
Abstract #P749
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Myelofibrosis
Patient characteristics, treatment
patterns, and health outcomes in a real-world population of
patients with myelofibrosis treated with fedratinib.
Francesco Passamonti
Poster
Abstract #P1034
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Fedratinib inhibits immune evasion and
restores B cell maturation: Biomarker analysis from the FREEDOM2
study.
Claire Harrison
Poster
Abstract #P1020
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Non-Hodgkin Lymphoma (includes
DLBCL, LBCL, FL, MCL, etc.)
Safety and efficacy of golcadomide, a
potential first-in-class CELMOD agent ± rituximab in a phase 1/2
open-label study of patients with relapsed/refractory (r/r)
follicular lymphoma (FL).
Julio Chavez
Poster
Abstract #P1132
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Golcadomide (Golca [CC-99282]), a novel
CELMoD agent, plus R-CHOP in patients (pts) with untreated
aggressive B-cell lymphoma (A-BCL): Updated safety and 12-month
efficacy results.
Marc Hoffmann
Oral
Abstract #S235
Friday, June 14, 2024
9:45 AM - 11:00 AM (14:45 - 16:00 CET)
Lisocabtagene maraleucel versus standard
of care with salvage chemotherapy followed by ASCT as second-line
treatment in patients with R/R large b-cell lymphoma: 3-year follow
up of TRANSFORM.
Jeremy Abramson
Oral
Abstract #S272
Sunday, June 16, 2024
6:30 AM - 7:45 AM (11:30 - 12:45 CET)
Subgroup analyses in patients with R/R MCL
treated with lisocabtagene maraleucel by prior lines of therapy and
response to bruton tyrosine kinase inhibitor from the TRANSCEND NHL
001 MCL cohort.
Manali Kamdar
Poster
Abstract #P1126
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Thalassemia (Alpha or Beta)
Safety data from the dose-finding cohorts:
a phase 2A study of luspatercept in pediatric patients with
βeta-thalassemia.
Antonis Kattamis
Poster
Abstract #P1516
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
Characterizing patterns of transfusion
burden (TB) reduction in patients (pts) with transfusion-dependent
(TD) βeta-thalassemia treated with luspatercept in the BELIEVE
trial.
Kevin Kuo
Poster
Abstract #P1522
Friday, June 14, 2024
1:00 PM - 2:00 PM (18:00 - 19:00 CET)
All EHA abstracts, except late-breaking abstracts, will be
available at 10:00 AM EDT on May 14. All late-breaking abstracts
will be available at 10:00 AM EDT on June 3.
Bristol Myers Squibb: Creating a Better
Future for People with Cancer
Bristol Myers Squibb is inspired by a single vision —
transforming patients’ lives through science. The goal of the
company’s cancer research is to deliver medicines that offer each
patient a better, healthier life and to make cure a possibility.
Building on a legacy across a broad range of cancers that have
changed survival expectations for many, Bristol Myers Squibb
researchers are exploring new frontiers in personalized medicine
and, through innovative digital platforms, are turning data into
insights that sharpen their focus. Deep understanding of causal
human biology, cutting-edge capabilities and differentiated
research platforms uniquely position the company to approach cancer
from every angle.
Cancer can have a relentless grasp on many parts of a patient’s
life, and Bristol Myers Squibb is committed to taking actions to
address all aspects of care, from diagnosis to survivorship. As a
leader in cancer care, Bristol Myers Squibb is working to empower
all people with cancer to have a better future.
OPDIVO
INDICATIONS
OPDIVO® (nivolumab), as a single agent, is indicated for the
treatment of adult and pediatric patients 12 years and older with
unresectable or metastatic melanoma.
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the treatment of adult and pediatric patients 12
years and older with unresectable or metastatic melanoma.
OPDIVO® is indicated for the adjuvant treatment of adult and
pediatric patients 12 years and older with completely resected
Stage IIB, Stage IIC, Stage III, or Stage IV melanoma.
OPDIVO® (nivolumab), in combination with platinum-doublet
chemotherapy, is indicated as neoadjuvant treatment of adult
patients with resectable (tumors ≥4 cm or node positive) non-small
cell lung cancer (NSCLC).
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the first-line treatment of adult patients with
metastatic non-small cell lung cancer (NSCLC) whose tumors express
PD-L1 (≥1%) as determined by an FDA-approved test, with no EGFR or
ALK genomic tumor aberrations.
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab)
and 2 cycles of platinum-doublet chemotherapy, is indicated for the
first-line treatment of adult patients with metastatic or recurrent
non-small cell lung cancer (NSCLC), with no EGFR or ALK genomic
tumor aberrations.
OPDIVO® (nivolumab) is indicated for the treatment of adult
patients with metastatic non-small cell lung cancer (NSCLC) with
progression on or after platinum-based chemotherapy. Patients with
EGFR or ALK genomic tumor aberrations should have disease
progression on FDA-approved therapy for these aberrations prior to
receiving OPDIVO.
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the first-line treatment of adult patients with
unresectable malignant pleural mesothelioma (MPM).
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the first-line treatment of adult patients with
intermediate or poor risk advanced renal cell carcinoma (RCC).
OPDIVO® (nivolumab), in combination with cabozantinib, is
indicated for the first-line treatment of adult patients with
advanced renal cell carcinoma (RCC).
OPDIVO® (nivolumab) is indicated for the treatment of adult
patients with advanced renal cell carcinoma (RCC) who have received
prior anti-angiogenic therapy.
OPDIVO® (nivolumab) is indicated for the treatment of adult
patients with classical Hodgkin lymphoma (cHL) that has relapsed or
progressed after autologous hematopoietic stem cell transplantation
(HSCT) and brentuximab vedotin or after 3 or more lines of systemic
therapy that includes autologous HSCT. This indication is approved
under accelerated approval based on overall response rate.
Continued approval for this indication may be contingent upon
verification and description of clinical benefit in confirmatory
trials.
OPDIVO® (nivolumab) is indicated for the treatment of adult
patients with recurrent or metastatic squamous cell carcinoma of
the head and neck (SCCHN) with disease progression on or after
platinum-based therapy.
OPDIVO® (nivolumab) is indicated for the treatment of adult
patients with locally advanced or metastatic urothelial carcinoma
who have disease progression during or following
platinum-containing chemotherapy or have disease progression within
12 months of neoadjuvant or adjuvant treatment with
platinum-containing chemotherapy.
OPDIVO® (nivolumab), as a single agent, is indicated for the
adjuvant treatment of adult patients with urothelial carcinoma (UC)
who are at high risk of recurrence after undergoing radical
resection of UC.
OPDIVO® (nivolumab), in combination with cisplatin and
gemcitabine, is indicated as first-line treatment for adult
patients with unresectable or metastatic urothelial carcinoma.
OPDIVO® (nivolumab), as a single agent, is indicated for the
treatment of adult and pediatric (12 years and older) patients with
microsatellite instability-high (MSI-H) or mismatch repair
deficient (dMMR) metastatic colorectal cancer (CRC) that has
progressed following treatment with a fluoropyrimidine,
oxaliplatin, and irinotecan. This indication is approved under
accelerated approval based on overall response rate and duration of
response. Continued approval for this indication may be contingent
upon verification and description of clinical benefit in
confirmatory trials.
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the treatment of adults and pediatric patients 12
years and older with microsatellite instability-high (MSI-H) or
mismatch repair deficient (dMMR) metastatic colorectal cancer (CRC)
that has progressed following treatment with a fluoropyrimidine,
oxaliplatin, and irinotecan. This indication is approved under
accelerated approval based on overall response rate and duration of
response. Continued approval for this indication may be contingent
upon verification and description of clinical benefit in
confirmatory trials.
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the treatment of adult patients with
hepatocellular carcinoma (HCC) who have been previously treated
with sorafenib. This indication is approved under accelerated
approval based on overall response rate and duration of response.
Continued approval for this indication may be contingent upon
verification and description of clinical benefit in the
confirmatory trials.
OPDIVO® (nivolumab) is indicated for the treatment of adult
patients with unresectable advanced, recurrent or metastatic
esophageal squamous cell carcinoma (ESCC) after prior
fluoropyrimidine- and platinum-based chemotherapy.
OPDIVO® (nivolumab) is indicated for the adjuvant treatment of
completely resected esophageal or gastroesophageal junction cancer
with residual pathologic disease in adult patients who have
received neoadjuvant chemoradiotherapy (CRT).
OPDIVO® (nivolumab), in combination with fluoropyrimidine- and
platinum-containing chemotherapy, is indicated for the first-line
treatment of adult patients with unresectable advanced or
metastatic esophageal squamous cell carcinoma (ESCC).
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the first-line treatment of adult patients with
unresectable advanced or metastatic esophageal squamous cell
carcinoma (ESCC).
OPDIVO® (nivolumab), in combination with fluoropyrimidine- and
platinum- containing chemotherapy, is indicated for the treatment
of adult patients with advanced or metastatic gastric cancer,
gastroesophageal junction cancer, and esophageal
adenocarcinoma.
IMPORTANT SAFETY
INFORMATION
Severe and Fatal Immune-Mediated Adverse Reactions
Immune-mediated adverse reactions listed herein may not include
all possible severe and fatal immune- mediated adverse
reactions.
Immune-mediated adverse reactions, which may be severe or fatal,
can occur in any organ system or tissue. While immune-mediated
adverse reactions usually manifest during treatment, they can also
occur after discontinuation of OPDIVO or YERVOY. Early
identification and management are essential to ensure safe use of
OPDIVO and YERVOY. Monitor for signs and symptoms that may be
clinical manifestations of underlying immune-mediated adverse
reactions. Evaluate clinical chemistries including liver enzymes,
creatinine, adrenocorticotropic hormone (ACTH) level, and thyroid
function at baseline and periodically during treatment with OPDIVO
and before each dose of YERVOY. In cases of suspected
immune-mediated adverse reactions, initiate appropriate workup to
exclude alternative etiologies, including infection. Institute
medical management promptly, including specialty consultation as
appropriate.
Withhold or permanently discontinue OPDIVO and YERVOY depending
on severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information). In general, if OPDIVO
or YERVOY interruption or discontinuation is required, administer
systemic corticosteroid therapy (1 to 2 mg/kg/day prednisone or
equivalent) until improvement to Grade 1 or less. Upon improvement
to Grade 1 or less, initiate corticosteroid taper and continue to
taper over at least 1 month. Consider administration of other
systemic immunosuppressants in patients whose immune-mediated
adverse reactions are not controlled with corticosteroid therapy.
Toxicity management guidelines for adverse reactions that do not
necessarily require systemic steroids (e.g., endocrinopathies and
dermatologic reactions) are discussed below.
Immune-Mediated Pneumonitis
OPDIVO and YERVOY can cause immune-mediated pneumonitis. The
incidence of pneumonitis is higher in patients who have received
prior thoracic radiation. In patients receiving OPDIVO monotherapy,
immune- mediated pneumonitis occurred in 3.1% (61/1994) of
patients, including Grade 4 (<0.1%), Grade 3 (0.9%), and Grade 2
(2.1%). In patients receiving OPDIVO 1 mg/kg with YERVOY 3 mg/kg
every 3 weeks, immune- mediated pneumonitis occurred in 7% (31/456)
of patients, including Grade 4 (0.2%), Grade 3 (2.0%), and Grade 2
(4.4%). In patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg
every 3 weeks, immune- mediated pneumonitis occurred in 3.9%
(26/666) of patients, including Grade 3 (1.4%) and Grade 2 (2.6%).
In NSCLC patients receiving OPDIVO 3 mg/kg every 2 weeks with
YERVOY 1 mg/kg every 6 weeks, immune- mediated pneumonitis occurred
in 9% (50/576) of patients, including Grade 4 (0.5%), Grade 3
(3.5%), and Grade 2 (4.0%). Four patients (0.7%) died due to
pneumonitis.
In Checkmate 205 and 039, pneumonitis, including interstitial
lung disease, occurred in 6.0% (16/266) of patients receiving
OPDIVO. Immune-mediated pneumonitis occurred in 4.9% (13/266) of
patients receiving OPDIVO, including Grade 3 (n=1) and Grade 2
(n=12).
Immune-Mediated Colitis
OPDIVO and YERVOY can cause immune-mediated colitis, which may
be fatal. A common symptom included in the definition of colitis
was diarrhea. Cytomegalovirus (CMV) infection/reactivation has been
reported in patients with corticosteroid-refractory immune-mediated
colitis. In cases of corticosteroid-refractory colitis, consider
repeating infectious workup to exclude alternative etiologies. In
patients receiving OPDIVO monotherapy, immune-mediated colitis
occurred in 2.9% (58/1994) of patients, including Grade 3 (1.7%)
and Grade 2 (1%).
In patients receiving OPDIVO 1 mg/kg with YERVOY 3 mg/kg every 3
weeks, immune-mediated colitis occurred in 25% (115/456) of
patients, including Grade 4 (0.4%), Grade 3 (14%) and Grade 2 (8%).
In patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3
weeks, immune-mediated colitis occurred in 9% (60/666) of patients,
including Grade 3 (4.4%) and Grade 2 (3.7%).
Immune-Mediated Hepatitis and
Hepatotoxicity
OPDIVO and YERVOY can cause immune-mediated hepatitis. In
patients receiving OPDIVO monotherapy, immune-mediated hepatitis
occurred in 1.8% (35/1994) of patients, including Grade 4 (0.2%),
Grade 3 (1.3%), and Grade 2 (0.4%).
In patients receiving OPDIVO 1 mg/kg with YERVOY 3 mg/kg every 3
weeks, immune-mediated hepatitis occurred in 15% (70/456) of
patients, including Grade 4 (2.4%), Grade 3 (11%), and Grade 2
(1.8%). In patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg
every 3 weeks, immune-mediated hepatitis occurred in 7% (48/666) of
patients, including Grade 4 (1.2%), Grade 3 (4.9%), and Grade 2
(0.4%).
OPDIVO in combination with cabozantinib can cause hepatic
toxicity with higher frequencies of Grade 3 and 4 ALT and AST
elevations compared to OPDIVO alone. Consider more frequent
monitoring of liver enzymes as compared to when the drugs are
administered as single agents. In patients receiving OPDIVO and
cabozantinib, Grades 3 and 4 increased ALT or AST were seen in 11%
of patients.
Immune-Mediated
Endocrinopathies
OPDIVO and YERVOY can cause primary or secondary adrenal
insufficiency, immune-mediated hypophysitis, immune-mediated
thyroid disorders, and Type 1 diabetes mellitus, which can present
with diabetic ketoacidosis. Withhold OPDIVO and YERVOY depending on
severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information). For Grade 2 or higher
adrenal insufficiency, initiate symptomatic treatment, including
hormone replacement as clinically indicated. Hypophysitis can
present with acute symptoms associated with mass effect such as
headache, photophobia, or visual field defects. Hypophysitis can
cause hypopituitarism; initiate hormone replacement as clinically
indicated. Thyroiditis can present with or without endocrinopathy.
Hypothyroidism can follow hyperthyroidism; initiate hormone
replacement or medical management as clinically indicated. Monitor
patients for hyperglycemia or other signs and symptoms of diabetes;
initiate treatment with insulin as clinically indicated.
In patients receiving OPDIVO monotherapy, adrenal insufficiency
occurred in 1% (20/1994), including Grade 3 (0.4%) and Grade 2
(0.6%). In patients receiving OPDIVO 1 mg/kg with YERVOY 3 mg/kg
every 3 weeks, adrenal insufficiency occurred in 8% (35/456),
including Grade 4 (0.2%), Grade 3 (2.4%), and Grade 2 (4.2%). In
patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3
weeks, adrenal insufficiency occurred in 7% (48/666) of patients,
including Grade 4 (0.3%), Grade 3 (2.5%), and Grade 2 (4.1%). In
patients receiving OPDIVO and cabozantinib, adrenal insufficiency
occurred in 4.7% (15/320) of patients, including Grade 3 (2.2%) and
Grade 2 (1.9%).
In patients receiving OPDIVO monotherapy, hypophysitis occurred
in 0.6% (12/1994) of patients, including Grade 3 (0.2%) and Grade 2
(0.3%).
In patients receiving OPDIVO 1 mg/kg with YERVOY 3 mg/kg every 3
weeks, hypophysitis occurred in 9% (42/456), including Grade 3
(2.4%) and Grade 2 (6%). In patients receiving OPDIVO 3 mg/kg with
YERVOY 1 mg/kg every 3 weeks, hypophysitis occurred in 4.4%
(29/666) of patients, including Grade 4 (0.3%), Grade 3 (2.4%), and
Grade 2 (0.9%).
In patients receiving OPDIVO monotherapy, thyroiditis occurred
in 0.6% (12/1994) of patients, including Grade 2 (0.2%). In
patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3
weeks, thyroiditis occurred in 2.7% (22/666) of patients, including
Grade 3 (4.5%) and Grade 2 (2.2%).
In patients receiving OPDIVO monotherapy, hyperthyroidism
occurred in 2.7% (54/1994) of patients, including Grade 3
(<0.1%) and Grade 2 (1.2%). In patients receiving OPDIVO 1 mg/kg
with YERVOY 3 mg/kg every 3 weeks, hyperthyroidism occurred in 9%
(42/456) of patients, including Grade 3 (0.9%) and Grade 2 (4.2%).
In patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3
weeks, hyperthyroidism occurred in 12% (80/666) of patients,
including Grade 3 (0.6%) and Grade 2 (4.5%).
In patients receiving OPDIVO monotherapy, hypothyroidism
occurred in 8% (163/1994) of patients, including Grade 3 (0.2%) and
Grade 2 (4.8%). In patients receiving OPDIVO 1 mg/kg with YERVOY 3
mg/kg every 3 weeks, hypothyroidism occurred in 20% (91/456) of
patients, including Grade 3 (0.4%) and Grade 2 (11%). In patients
receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3 weeks,
hypothyroidism occurred in 18% (122/666) of patients, including
Grade 3 (0.6%) and Grade 2 (11%).
In patients receiving OPDIVO monotherapy, diabetes occurred in
0.9% (17/1994) of patients, including Grade 3 (0.4%) and Grade 2
(0.3%), and 2 cases of diabetic ketoacidosis. In patients receiving
OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3 weeks, diabetes occurred
in 2.7% (15/666) of patients, including Grade 4 (0.6%), Grade 3
(0.3%), and Grade 2 (0.9%).
Immune-Mediated Nephritis with Renal
Dysfunction
OPDIVO and YERVOY can cause immune-mediated nephritis. In
patients receiving OPDIVO monotherapy, immune-mediated nephritis
and renal dysfunction occurred in 1.2% (23/1994) of patients,
including Grade 4 (<0.1%), Grade 3 (0.5%), and Grade 2 (0.6%).
In patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3
weeks, immune-mediated nephritis with renal dysfunction occurred in
4.1% (27/666) of patients, including Grade 4 (0.6%), Grade 3
(1.1%), and Grade 2 (2.2%).
Immune-Mediated Dermatologic Adverse
Reactions
OPDIVO can cause immune-mediated rash or dermatitis. Exfoliative
dermatitis, including Stevens-Johnson syndrome (SJS), toxic
epidermal necrolysis (TEN), and drug rash with eosinophilia and
systemic symptoms (DRESS) has occurred with PD-1/PD-L1 blocking
antibodies. Topical emollients and/or topical corticosteroids may
be adequate to treat mild to moderate nonexfoliative rashes.
YERVOY can cause immune-mediated rash or dermatitis, including
bullous and exfoliative dermatitis, SJS, TEN, and DRESS. Topical
emollients and/or topical corticosteroids may be adequate to treat
mild to moderate non-bullous/exfoliative rashes.
Withhold or permanently discontinue OPDIVO and YERVOY depending
on severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information).
In patients receiving OPDIVO monotherapy, immune-mediated rash
occurred in 9% (171/1994) of patients, including Grade 3 (1.1%) and
Grade 2 (2.2%). In patients receiving OPDIVO 1 mg/kg with YERVOY 3
mg/kg every 3 weeks, immune-mediated rash occurred in 28% (127/456)
of patients, including Grade 3 (4.8%) and Grade 2 (10%). In
patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3
weeks, immune-mediated rash occurred in 16% (108/666) of patients,
including Grade 3 (3.5%) and Grade 2 (4.2%).
Other Immune-Mediated Adverse
Reactions
The following clinically significant immune-mediated adverse
reactions occurred at an incidence of <1% (unless otherwise
noted) in patients who received OPDIVO monotherapy or OPDIVO in
combination with YERVOY or were reported with the use of other
PD-1/PD-L1 blocking antibodies. Severe or fatal cases have been
reported for some of these adverse reactions: cardiac/vascular:
myocarditis, pericarditis, vasculitis; nervous system: meningitis,
encephalitis, myelitis and demyelination, myasthenic
syndrome/myasthenia gravis (including exacerbation), Guillain-Barré
syndrome, nerve paresis, autoimmune neuropathy; ocular: uveitis,
iritis, and other ocular inflammatory toxicities can occur;
gastrointestinal: pancreatitis to include increases in serum
amylase and lipase levels, gastritis, duodenitis; musculoskeletal
and connective tissue: myositis/polymyositis, rhabdomyolysis, and
associated sequelae including renal failure, arthritis, polymyalgia
rheumatica; endocrine: hypoparathyroidism; other
(hematologic/immune): hemolytic anemia, aplastic anemia,
hemophagocytic lymphohistiocytosis (HLH), systemic inflammatory
response syndrome, histiocytic necrotizing lymphadenitis (Kikuchi
lymphadenitis), sarcoidosis, immune thrombocytopenic purpura, solid
organ transplant rejection, other transplant (including corneal
graft) rejection.
In addition to the immune-mediated adverse reactions listed
above, across clinical trials of YERVOY monotherapy or in
combination with OPDIVO, the following clinically significant
immune-mediated adverse reactions, some with fatal outcome,
occurred in <1% of patients unless otherwise specified: nervous
system: autoimmune neuropathy (2%), myasthenic syndrome/myasthenia
gravis, motor dysfunction; cardiovascular: angiopathy, temporal
arteritis; ocular: blepharitis, episcleritis, orbital myositis,
scleritis; gastrointestinal: pancreatitis (1.3%); other
(hematologic/immune): conjunctivitis, cytopenias (2.5%),
eosinophilia (2.1%), erythema multiforme, hypersensitivity
vasculitis, neurosensory hypoacusis, psoriasis.
Some ocular IMAR cases can be associated with retinal
detachment. Various grades of visual impairment, including
blindness, can occur. If uveitis occurs in combination with other
immune-mediated adverse reactions, consider a
Vogt-Koyanagi-Harada-like syndrome, which has been observed in
patients receiving OPDIVO and YERVOY, as this may require treatment
with systemic corticosteroids to reduce the risk of permanent
vision loss.
Infusion-Related Reactions
OPDIVO and YERVOY can cause severe infusion-related reactions.
Discontinue OPDIVO and YERVOY in patients with severe (Grade 3) or
life-threatening (Grade 4) infusion-related reactions. Interrupt or
slow the rate of infusion in patients with mild (Grade 1) or
moderate (Grade 2) infusion-related reactions. In patients
receiving OPDIVO monotherapy as a 60-minute infusion,
infusion-related reactions occurred in 6.4% (127/1994) of patients.
In a separate trial in which patients received OPDIVO monotherapy
as a 60-minute infusion or a 30- minute infusion, infusion-related
reactions occurred in 2.2% (8/368) and 2.7% (10/369) of patients,
respectively. Additionally, 0.5% (2/368) and 1.4% (5/369) of
patients, respectively, experienced adverse reactions within 48
hours of infusion that led to dose delay, permanent discontinuation
or withholding of OPDIVO. In melanoma patients receiving OPDIVO 1
mg/kg with YERVOY 3 mg/kg every 3 weeks, infusion-related reactions
occurred in 2.5% (10/407) of patients. In HCC patients receiving
OPDIVO 1 mg/kg with YERVOY 3 mg/kg every 3 weeks, infusion-related
reactions occurred in 8% (4/49) of patients. In RCC patients
receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3 weeks,
infusion-related reactions occurred in 5.1% (28/547) of patients.
In MSI-H/dMMR mCRC patients receiving OPDIVO 3 mg/kg with YERVOY 1
mg/kg every 3 weeks, infusion-related reactions occurred in 4.2%
(5/119) of patients. In MPM patients receiving OPDIVO 3 mg/kg every
2 weeks with YERVOY 1 mg/kg every 6 weeks, infusion-related
reactions occurred in 12% (37/300) of patients.
Complications of Allogeneic Hematopoietic Stem Cell
Transplantation
Fatal and other serious complications can occur in patients who
receive allogeneic hematopoietic stem cell transplantation (HSCT)
before or after being treated with OPDIVO or YERVOY.
Transplant-related complications include hyperacute
graft-versus-host-disease (GVHD), acute GVHD, chronic GVHD, hepatic
veno-occlusive disease (VOD) after reduced intensity conditioning,
and steroid-requiring febrile syndrome (without an identified
infectious cause). These complications may occur despite
intervening therapy between OPDIVO or YERVOY and allogeneic
HSCT.
Follow patients closely for evidence of transplant-related
complications and intervene promptly. Consider the benefit versus
risks of treatment with OPDIVO and YERVOY prior to or after an
allogeneic HSCT.
Embryo-Fetal Toxicity
Based on its mechanism of action and findings from animal
studies, OPDIVO and YERVOY can cause fetal harm when administered
to a pregnant woman. The effects of YERVOY are likely to be greater
during the second and third trimesters of pregnancy. Advise
pregnant women of the potential risk to a fetus. Advise females of
reproductive potential to use effective contraception during
treatment with OPDIVO and YERVOY and for at least 5 months after
the last dose.
Increased Mortality in Patients with Multiple Myeloma when
OPDIVO is Added to a Thalidomide Analogue and Dexamethasone
In randomized clinical trials in patients with multiple myeloma,
the addition of OPDIVO to a thalidomide analogue plus dexamethasone
resulted in increased mortality. Treatment of patients with
multiple myeloma with a PD-1 or PD-L1 blocking antibody in
combination with a thalidomide analogue plus dexamethasone is not
recommended outside of controlled clinical trials.
Lactation
There are no data on the presence of OPDIVO or YERVOY in human
milk, the effects on the breastfed child, or the effects on milk
production. Because of the potential for serious adverse reactions
in breastfed children, advise women not to breastfeed during
treatment and for 5 months after the last dose.
Serious Adverse Reactions
In Checkmate 037, serious adverse reactions occurred in 41% of
patients receiving OPDIVO (n=268). Grade 3 and 4 adverse reactions
occurred in 42% of patients receiving OPDIVO. The most frequent
Grade 3 and 4 adverse drug reactions reported in 2% to <5% of
patients receiving OPDIVO were abdominal pain, hyponatremia,
increased aspartate aminotransferase, and increased lipase. In
Checkmate 066, serious adverse reactions occurred in 36% of
patients receiving OPDIVO (n=206). Grade 3 and 4 adverse reactions
occurred in 41% of patients receiving OPDIVO. The most frequent
Grade 3 and 4 adverse reactions reported in ≥2% of patients
receiving OPDIVO were gamma-glutamyltransferase increase (3.9%) and
diarrhea (3.4%). In Checkmate 067, serious adverse reactions (74%
and 44%), adverse reactions leading to permanent discontinuation
(47% and 18%) or to dosing delays (58% and 36%), and Grade 3 or 4
adverse reactions (72% and 51%) all occurred more frequently in the
OPDIVO plus YERVOY arm (n=313) relative to the OPDIVO arm (n=313).
The most frequent (≥10%) serious adverse reactions in the OPDIVO
plus YERVOY arm and the OPDIVO arm, respectively, were diarrhea
(13% and 2.2%), colitis (10% and 1.9%), and pyrexia (10% and 1.0%).
In Checkmate 238, serious adverse reactions occurred in 18% of
patients receiving OPDIVO (n=452). Grade 3 or 4 adverse reactions
occurred in 25% of OPDIVO-treated patients (n=452). The most
frequent Grade 3 and 4 adverse reactions reported in ≥2% of
OPDIVO-treated patients were diarrhea and increased lipase and
amylase. In Checkmate 816, serious adverse reactions occurred in
30% of patients (n=176) who were treated with OPDIVO in combination
with platinum-doublet chemotherapy. Serious adverse reactions in
>2% included pneumonia and vomiting. No fatal adverse reactions
occurred in patients who received OPDIVO in combination with
platinum-doublet chemotherapy. In Checkmate 227, serious adverse
reactions occurred in 58% of patients (n=576). The most frequent
(≥2%) serious adverse reactions were pneumonia, diarrhea/colitis,
pneumonitis, hepatitis, pulmonary embolism, adrenal insufficiency,
and hypophysitis. Fatal adverse reactions occurred in 1.7% of
patients; these included events of pneumonitis (4 patients),
myocarditis, acute kidney injury, shock, hyperglycemia,
multi-system organ failure, and renal failure. In Checkmate 9LA,
serious adverse reactions occurred in 57% of patients (n=358). The
most frequent (>2%) serious adverse reactions were pneumonia,
diarrhea, febrile neutropenia, anemia, acute kidney injury,
musculoskeletal pain, dyspnea, pneumonitis, and respiratory
failure. Fatal adverse reactions occurred in 7 (2%) patients, and
included hepatic toxicity, acute renal failure, sepsis,
pneumonitis, diarrhea with hypokalemia, and massive hemoptysis in
the setting of thrombocytopenia. In Checkmate 017 and 057, serious
adverse reactions occurred in 46% of patients receiving OPDIVO
(n=418). The most frequent serious adverse reactions reported in
≥2% of patients receiving OPDIVO were pneumonia, pulmonary
embolism, dyspnea, pyrexia, pleural effusion, pneumonitis, and
respiratory failure. In Checkmate 057, fatal adverse reactions
occurred; these included events of infection (7 patients, including
one case of Pneumocystis jirovecii pneumonia), pulmonary embolism
(4 patients), and limbic encephalitis (1 patient). In Checkmate
743, serious adverse reactions occurred in 54% of patients
receiving OPDIVO plus YERVOY. The most frequent serious adverse
reactions reported in ≥2% of patients were pneumonia, pyrexia,
diarrhea, pneumonitis, pleural effusion, dyspnea, acute kidney
injury, infusion-related reaction, musculoskeletal pain, and
pulmonary embolism. Fatal adverse reactions occurred in 4 (1.3%)
patients and included pneumonitis, acute heart failure, sepsis, and
encephalitis. In Checkmate 214, serious adverse reactions occurred
in 59% of patients receiving OPDIVO plus YERVOY (n=547). The most
frequent serious adverse reactions reported in ≥2% of patients were
diarrhea, pyrexia, pneumonia, pneumonitis, hypophysitis, acute
kidney injury, dyspnea, adrenal insufficiency, and colitis. In
Checkmate 9ER, serious adverse reactions occurred in 48% of
patients receiving OPDIVO and cabozantinib (n=320). The most
frequent serious adverse reactions reported in ≥2% of patients were
diarrhea, pneumonia, pneumonitis, pulmonary embolism, urinary tract
infection, and hyponatremia. Fatal intestinal perforations occurred
in 3 (0.9%) patients. In Checkmate 025, serious adverse reactions
occurred in 47% of patients receiving OPDIVO (n=406). The most
frequent serious adverse reactions reported in ≥2% of patients were
acute kidney injury, pleural effusion, pneumonia, diarrhea, and
hypercalcemia. In Checkmate 205 and 039, adverse reactions leading
to discontinuation occurred in 7% and dose delays due to adverse
reactions occurred in 34% of patients (n=266). Serious adverse
reactions occurred in 26% of patients. The most frequent serious
adverse reactions reported in ≥1% of patients were pneumonia,
infusion-related reaction, pyrexia, colitis or diarrhea, pleural
effusion, pneumonitis, and rash. Eleven patients died from causes
other than disease progression: 3 from adverse reactions within 30
days of the last OPDIVO dose, 2 from infection 8 to 9 months after
completing OPDIVO, and 6 from complications of allogeneic HSCT. In
Checkmate 141, serious adverse reactions occurred in 49% of
patients receiving OPDIVO (n=236). The most frequent serious
adverse reactions reported in ≥2% of patients receiving OPDIVO were
pneumonia, dyspnea, respiratory failure, respiratory tract
infection, and sepsis. In Checkmate 275, serious adverse reactions
occurred in 54% of patients receiving OPDIVO (n=270). The most
frequent serious adverse reactions reported in ≥2% of patients
receiving OPDIVO were urinary tract infection, sepsis, diarrhea,
small intestine obstruction, and general physical health
deterioration. In Checkmate 274, serious adverse reactions occurred
in 30% of patients receiving OPDIVO (n=351). The most frequent
serious adverse reaction reported in ≥2% of patients receiving
OPDIVO was urinary tract infection. Fatal adverse reactions
occurred in 1% of patients; these included events of pneumonitis
(0.6%). In Checkmate 901, serious adverse reactions occurred in 48%
of patients receiving OPDIVO in combination with chemotherapy. The
most frequent serious adverse reactions reporting in ≥2% of
patients who received OPDIVO with chemotherapy were urinary tract
infection (4.9%), acute kidney injury (4.3%), anemia (3%),
pulmonary embolism (2.6%), sepsis (2.3%), and platelet count
decreased (2.3%). Fatal adverse reactions occurred in 3.6% of
patients who received OPDIVO in combination with chemotherapy;
these included sepsis (1%). OPDIVO and/or chemotherapy were
discontinued in 30% of patients and were delayed in 67% of patients
for an adverse reaction. In Checkmate 142 in MSI-H/dMMR mCRC
patients receiving OPDIVO with YERVOY (n=119), serious adverse
reactions occurred in 47% of patients. The most frequent serious
adverse reactions reported in ≥2% of patients were
colitis/diarrhea, hepatic events, abdominal pain, acute kidney
injury, pyrexia, and dehydration. In Checkmate 040, serious adverse
reactions occurred in 59% of patients receiving OPDIVO with YERVOY
(n=49). Serious adverse reactions reported in ≥4% of patients were
pyrexia, diarrhea, anemia, increased AST, adrenal insufficiency,
ascites, esophageal varices hemorrhage, hyponatremia, increased
blood bilirubin, and pneumonitis. In Attraction-3, serious adverse
reactions occurred in 38% of patients receiving OPDIVO (n=209).
Serious adverse reactions reported in ≥2% of patients who received
OPDIVO were pneumonia, esophageal fistula, interstitial lung
disease, and pyrexia. The following fatal adverse reactions
occurred in patients who received OPDIVO: interstitial lung disease
or pneumonitis (1.4%), pneumonia (1.0%), septic shock (0.5%),
esophageal fistula (0.5%), gastrointestinal hemorrhage (0.5%),
pulmonary embolism (0.5%), and sudden death (0.5%). In Checkmate
577, serious adverse reactions occurred in 33% of patients
receiving OPDIVO (n=532). A serious adverse reaction reported in
≥2% of patients who received OPDIVO was pneumonitis. A fatal
reaction of myocardial infarction occurred in one patient who
received OPDIVO. In Checkmate 648, serious adverse reactions
occurred in 62% of patients receiving OPDIVO in combination with
chemotherapy (n=310). The most frequent serious adverse reactions
reported in ≥2% of patients who received OPDIVO with chemotherapy
were pneumonia (11%), dysphagia (7%), esophageal stenosis (2.9%),
acute kidney injury (2.9%), and pyrexia (2.3%). Fatal adverse
reactions occurred in 5 (1.6%) patients who received OPDIVO in
combination with chemotherapy; these included pneumonitis,
pneumatosis intestinalis, pneumonia, and acute kidney injury. In
Checkmate 648, serious adverse reactions occurred in 69% of
patients receiving OPDIVO in combination with YERVOY (n=322). The
most frequent serious adverse reactions reported in ≥2% who
received OPDIVO in combination with YERVOY were pneumonia (10%),
pyrexia (4.3%), pneumonitis (4.0%), aspiration pneumonia (3.7%),
dysphagia (3.7%), hepatic function abnormal (2.8%), decreased
appetite (2.8%), adrenal insufficiency (2.5%), and dehydration
(2.5%). Fatal adverse reactions occurred in 5 (1.6%) patients who
received OPDIVO in combination with YERVOY; these included
pneumonitis, interstitial lung disease, pulmonary embolism, and
acute respiratory distress syndrome. In Checkmate 649, serious
adverse reactions occurred in 52% of patients treated with OPDIVO
in combination with chemotherapy (n=782). The most frequent serious
adverse reactions reported in ≥2% of patients treated with OPDIVO
in combination with chemotherapy were vomiting (3.7%), pneumonia
(3.6%), anemia (3.6%), pyrexia (2.8%), diarrhea (2.7%), febrile
neutropenia (2.6%), and pneumonitis (2.4%). Fatal adverse reactions
occurred in 16 (2.0%) patients who were treated with OPDIVO in
combination with chemotherapy; these included pneumonitis (4
patients), febrile neutropenia (2 patients), stroke (2 patients),
gastrointestinal toxicity, intestinal mucositis, septic shock,
pneumonia, infection, gastrointestinal bleeding, mesenteric vessel
thrombosis, and disseminated intravascular coagulation. In
Checkmate 76K, serious adverse reactions occurred in 18% of
patients receiving OPDIVO (n=524). Adverse reactions which resulted
in permanent discontinuation of OPDIVO in >1% of patients
included arthralgia (1.7%), rash (1.7%), and diarrhea (1.1%). A
fatal adverse reaction occurred in 1 (0.2%) patient (heart failure
and acute kidney injury). The most frequent Grade 3-4 lab
abnormalities reported in ≥1% of OPDIVO-treated patients were
increased lipase (2.9%), increased AST (2.2%), increased ALT
(2.1%), lymphopenia (1.1%), and decreased potassium (1.0%).
Common Adverse Reactions
In Checkmate 037, the most common adverse reaction (≥20%)
reported with OPDIVO (n=268) was rash (21%). In Checkmate 066, the
most common adverse reactions (≥20%) reported with OPDIVO (n=206)
vs dacarbazine (n=205) were fatigue (49% vs 39%), musculoskeletal
pain (32% vs 25%), rash (28% vs 12%), and pruritus (23% vs 12%). In
Checkmate 067, the most common (≥20%) adverse reactions in the
OPDIVO plus YERVOY arm (n=313) were fatigue (62%), diarrhea (54%),
rash (53%), nausea (44%), pyrexia (40%), pruritus (39%),
musculoskeletal pain (32%), vomiting (31%), decreased appetite
(29%), cough (27%), headache (26%), dyspnea (24%), upper
respiratory tract infection (23%), arthralgia (21%), and increased
transaminases (25%). In Checkmate 067, the most common (≥20%)
adverse reactions in the OPDIVO arm (n=313) were fatigue (59%),
rash (40%), musculoskeletal pain (42%), diarrhea (36%), nausea
(30%), cough (28%), pruritus (27%), upper respiratory tract
infection (22%), decreased appetite (22%), headache (22%),
constipation (21%), arthralgia (21%), and vomiting (20%). In
Checkmate 238, the most common adverse reactions (≥20%) reported in
OPDIVO-treated patients (n=452) vs ipilimumab-treated patients
(n=453) were fatigue (57% vs 55%), diarrhea (37% vs 55%), rash (35%
vs 47%), musculoskeletal pain (32% vs 27%), pruritus (28% vs 37%),
headache (23% vs 31%), nausea (23% vs 28%), upper respiratory
infection (22% vs 15%), and abdominal pain (21% vs 23%). The most
common immune-mediated adverse reactions were rash (16%),
diarrhea/colitis (6%), and hepatitis (3%). In Checkmate 816, the
most common (>20%) adverse reactions in the OPDIVO plus
chemotherapy arm (n=176) were nausea (38%), constipation (34%),
fatigue (26%), decreased appetite (20%), and rash (20%). In
Checkmate 227, the most common (≥20%) adverse reactions were
fatigue (44%), rash (34%), decreased appetite (31%),
musculoskeletal pain (27%), diarrhea/colitis (26%), dyspnea (26%),
cough (23%), hepatitis (21%), nausea (21%), and pruritus (21%). In
Checkmate 9LA, the most common (>20%) adverse reactions were
fatigue (49%), musculoskeletal pain (39%), nausea (32%), diarrhea
(31%), rash (30%), decreased appetite (28%), constipation (21%),
and pruritus (21%). In Checkmate 017 and 057, the most common
adverse reactions (≥20%) in patients receiving OPDIVO (n=418) were
fatigue, musculoskeletal pain, cough, dyspnea, and decreased
appetite. In Checkmate 743, the most common adverse reactions
(≥20%) in patients receiving OPDIVO plus YERVOY were fatigue (43%),
musculoskeletal pain (38%), rash (34%), diarrhea (32%), dyspnea
(27%), nausea (24%), decreased appetite (24%), cough (23%), and
pruritus (21%). In Checkmate 214, the most common adverse reactions
(≥20%) reported in patients treated with OPDIVO plus YERVOY (n=547)
were fatigue (58%), rash (39%), diarrhea (38%), musculoskeletal
pain (37%), pruritus (33%), nausea (30%), cough (28%), pyrexia
(25%), arthralgia (23%), decreased appetite (21%), dyspnea (20%),
and vomiting (20%). In Checkmate 9ER, the most common adverse
reactions (≥20%) in patients receiving OPDIVO and cabozantinib
(n=320) were diarrhea (64%), fatigue (51%), hepatotoxicity (44%),
palmar-plantar erythrodysaesthesia syndrome (40%), stomatitis
(37%), rash (36%), hypertension (36%), hypothyroidism (34%),
musculoskeletal pain (33%), decreased appetite (28%), nausea (27%),
dysgeusia (24%), abdominal pain (22%), cough (20%) and upper
respiratory tract infection (20%). In Checkmate 025, the most
common adverse reactions (≥20%) reported in patients receiving
OPDIVO (n=406) vs everolimus (n=397) were fatigue (56% vs 57%),
cough (34% vs 38%), nausea (28% vs 29%), rash (28% vs 36%), dyspnea
(27% vs 31%), diarrhea (25% vs 32%), constipation (23% vs 18%),
decreased appetite (23% vs 30%), back pain (21% vs 16%), and
arthralgia (20% vs 14%). In Checkmate 205 and 039, the most common
adverse reactions (≥20%) reported in patients receiving OPDIVO
(n=266) were upper respiratory tract infection (44%), fatigue
(39%), cough (36%), diarrhea (33%), pyrexia (29%), musculoskeletal
pain (26%), rash (24%), nausea (20%) and pruritus (20%). In
Checkmate 141, the most common adverse reactions (≥10%) in patients
receiving OPDIVO (n=236) were cough (14%) and dyspnea (14%) at a
higher incidence than investigator’s choice. In Checkmate 275, the
most common adverse reactions (≥20%) reported in patients receiving
OPDIVO (n=270) were fatigue (46%), musculoskeletal pain (30%),
nausea (22%), and decreased appetite (22%). In Checkmate 274, the
most common adverse reactions (≥20%) reported in patients receiving
OPDIVO (n=351) were rash (36%), fatigue (36%), diarrhea (30%),
pruritus (30%), musculoskeletal pain (28%), and urinary tract
infection (22%).In Checkmate 901, the most common adverse reactions
(≥20%) were nausea, fatigue, musculoskeletal pain, constipation,
decreased appetite, rash, vomiting, and peripheral neuropathy. In
Checkmate 142 in MSI-H/dMMR mCRC patients receiving OPDIVO as a
single agent (n=74), the most common adverse reactions (≥20%) were
fatigue (54%), diarrhea (43%), abdominal pain (34%), nausea (34%),
vomiting (28%), musculoskeletal pain (28%), cough (26%), pyrexia
(24%), rash (23%), constipation (20%), and upper respiratory tract
infection (20%). In Checkmate 142 in MSI-H/dMMR mCRC patients
receiving OPDIVO with YERVOY (n=119), the most common adverse
reactions (≥20%) were fatigue (49%), diarrhea (45%), pyrexia (36%),
musculoskeletal pain (36%), abdominal pain (30%), pruritus (28%),
nausea (26%), rash (25%), decreased appetite (20%), and vomiting
(20%). In Checkmate 040, the most common adverse reactions (≥20%)
in patients receiving OPDIVO with YERVOY (n=49), were rash (53%),
pruritus (53%), musculoskeletal pain (41%), diarrhea (39%), cough
(37%), decreased appetite (35%), fatigue (27%), pyrexia (27%),
abdominal pain (22%), headache (22%), nausea (20%), dizziness
(20%), hypothyroidism (20%), and weight decreased (20%). In
Attraction-3, the most common adverse reactions (≥20%) in
OPDIVO-treated patients (n=209) were rash (22%) and decreased
appetite (21%). In Checkmate 577, the most common adverse reactions
(≥20%) in patients receiving OPDIVO (n=532) were fatigue (34%),
diarrhea (29%), nausea (23%), rash (21%), musculoskeletal pain
(21%), and cough (20%). In Checkmate 648, the most common adverse
reactions (≥20%) in patients treated with OPDIVO in combination
with chemotherapy (n=310) were nausea (65%), decreased appetite
(51%), fatigue (47%), constipation (44%), stomatitis (44%),
diarrhea (29%), and vomiting (23%). In Checkmate 648, the most
common adverse reactions reported in ≥20% of patients treated with
OPDIVO in combination with YERVOY were rash (31%), fatigue (28%),
pyrexia (23%), nausea (22%), diarrhea (22%), and constipation
(20%). In Checkmate 649, the most common adverse reactions (≥20%)
in patients treated with OPDIVO in combination with chemotherapy
(n=782) were peripheral neuropathy (53%), nausea (48%), fatigue
(44%), diarrhea (39%), vomiting (31%), decreased appetite (29%),
abdominal pain (27%), constipation (25%), and musculoskeletal pain
(20%). In Checkmate 76K, the most common adverse reactions (≥20%)
reported with OPDIVO (n=524) were fatigue (36%), musculoskeletal
pain (30%), rash (28%), diarrhea (23%) and pruritis (20%).
Please see U.S. Full Prescribing Information for OPDIVO and
YERVOY.
Clinical Trials and Patient Populations
Checkmate 227—previously untreated metastatic non-small cell
lung cancer, in combination with YERVOY; Checkmate 9LA-previously
untreated recurrent or metastatic non-small cell lung cancer in
combination with YERVOY and 2 cycles of platinum-doublet
chemotherapy by histology; Checkmate 649-previously untreated
advanced or metastatic gastric cancer, gastroesophageal junction
and esophageal adenocarcinoma; Checkmate 577-adjuvant treatment of
esophageal or gastroesophageal junction cancer; Checkmate 238-
adjuvant treatment of patients with completely resected Stage III
or Stage IV melanoma; Checkmate 76K- adjuvant treatment of patients
12 years of age and older with completely resected Stage IIB or
Stage IIC melanoma; Checkmate 274-adjuvant treatment of urothelial
carcinoma; Checkmate 275-previously treated advanced or metastatic
urothelial carcinoma; Checkmate 142-MSI-H or dMMR metastatic
colorectal cancer, as a single agent or in combination with YERVOY;
Checkmate 142-MSI-H or dMMR metastatic colorectal cancer, as a
single agent or in combination with YERVOY; Attraction-3-esophageal
squamous cell carcinoma; Checkmate 648—previously untreated,
unresectable advanced recurrent or metastatic esophageal squamous
cell carcinoma; Checkmate 648—previously untreated, unresectable
advanced recurrent or metastatic esophageal squamous cell
carcinoma; Checkmate 040-hepatocellular carcinoma, in combination
with YERVOY; Checkmate 743-previously untreated unresectable
malignant pleural mesothelioma, in combination with YERVOY;
Checkmate 037-previously treated metastatic melanoma; Checkmate
066—previously untreated metastatic melanoma; Checkmate
067-previously untreated metastatic melanoma, as a single agent or
in combination with YERVOY; Checkmate 017-second-line treatment of
metastatic squamous non-small cell lung cancer; Checkmate
057-second-line treatment of metastatic non-squamous non-small cell
lung cancer; Checkmate 816-neoadjuvant non-small cell lung cancer,
in combination with platinum-doublet chemotherapy; Checkmate
901-Adult patients with unresectable or metastatic urothelial
carcinoma; Checkmate 141-recurrent or metastatic squamous cell
carcinoma of the head and neck; Checkmate 025-previously treated
renal cell carcinoma; Checkmate 214-previously untreated renal cell
carcinoma, in combination with YERVOY; Checkmate 9ER-previously
untreated renal cell carcinoma, in combination with cabozantinib;
Checkmate 205/039-classical Hodgkin lymphoma
OPDUALAG
INDICATION
Opdualag™ (nivolumab and relatlimab-rmbw) is indicated for the
treatment of adult and pediatric patients 12 years of age or older
with unresectable or metastatic melanoma.
IMPORTANT SAFETY
INFORMATION
Severe and Fatal Immune-Mediated Adverse Reactions
Immune-mediated adverse reactions (IMARs) listed herein may not
include all possible severe and fatal immune-mediated adverse
reactions.
IMARs which may be severe or fatal, can occur in any organ
system or tissue. IMARs can occur at any time after starting
treatment with a LAG-3 and PD-1/PD-L1 blocking antibodies. While
IMARs usually manifest during treatment, they can also occur after
discontinuation of Opdualag. Early identification and management of
IMARs are essential to ensure safe use. Monitor patients closely
for symptoms and signs that may be clinical manifestations of
underlying IMARs. Evaluate clinical chemistries including liver
enzymes, creatinine, and thyroid function at baseline and
periodically during treatment. In cases of suspected IMARs,
initiate appropriate workup to exclude alternative etiologies,
including infection. Institute medical management promptly,
including specialty consultation as appropriate.
Withhold or permanently discontinue Opdualag depending on
severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information). In general, if Opdualag
requires interruption or discontinuation, administer systemic
corticosteroid therapy (1 to 2 mg/kg/day prednisone or equivalent)
until improvement to Grade 1 or less. Upon improvement to Grade 1
or less, initiate corticosteroid taper and continue to taper over
at least 1 month. Consider administration of other systemic
immunosuppressants in patients whose IMARs are not controlled with
corticosteroid therapy. Toxicity management guidelines for adverse
reactions that do not necessarily require systemic steroids (e.g.,
endocrinopathies and dermatologic reactions) are discussed
below.
Immune-Mediated Pneumonitis
Opdualag can cause immune-mediated pneumonitis, which may be
fatal. In patients treated with other PD- 1/PD-L1 blocking
antibodies, the incidence of pneumonitis is higher in patients who
have received prior thoracic radiation. Immune-mediated pneumonitis
occurred in 3.7% (13/355) of patients receiving Opdualag, including
Grade 3 (0.6%), and Grade 2 (2.3%) adverse reactions. Pneumonitis
led to permanent discontinuation of Opdualag in 0.8% and
withholding of Opdualag in 1.4% of patients.
Immune-Mediated Colitis
Opdualag can cause immune-mediated colitis, defined as requiring
use of corticosteroids and no clear alternate etiology. A common
symptom included in the definition of colitis was diarrhea.
Cytomegalovirus infection/reactivation has been reported in
patients with corticosteroid-refractory immune-mediated colitis. In
cases of corticosteroid-refractory colitis, consider repeating
infectious workup to exclude alternative etiologies.
Immune-mediated diarrhea or colitis occurred in 7% (24/355) of
patients receiving Opdualag, including Grade 3 (1.1%) and Grade 2
(4.5%) adverse reactions. Colitis led to permanent discontinuation
of Opdualag in 2% and withholding of Opdualag in 2.8% of
patients.
Immune-Mediated Hepatitis
Opdualag can cause immune-mediated hepatitis, defined as
requiring the use of corticosteroids and no clear alternate
etiology.
Immune-mediated hepatitis occurred in 6% (20/355) of patients
receiving Opdualag, including Grade 4 (0.6%), Grade 3 (3.4%), and
Grade 2 (1.4%) adverse reactions. Hepatitis led to permanent
discontinuation of Opdualag in 1.7% and withholding of Opdualag in
2.3% of patients.
Immune-Mediated
Endocrinopathies
Opdualag can cause primary or secondary adrenal insufficiency,
hypophysitis, thyroid disorders, and Type 1 diabetes mellitus,
which can be present with diabetic ketoacidosis. Withhold or
permanently discontinue Opdualag depending on severity (please see
section 2 Dosage and Administration in the accompanying Full
Prescribing Information).
For Grade 2 or higher adrenal insufficiency, initiate
symptomatic treatment, including hormone replacement as clinically
indicated. In patients receiving Opdualag, adrenal insufficiency
occurred in 4.2% (15/355) of patients receiving Opdualag, including
Grade 3 (1.4%) and Grade 2 (2.5%) adverse reactions. Adrenal
insufficiency led to permanent discontinuation of Opdualag in 1.1%
and withholding of Opdualag in 0.8% of patients.
Hypophysitis can present with acute symptoms associated with
mass effect such as headache, photophobia, or visual field defects.
Hypophysitis can cause hypopituitarism; initiate hormone
replacement as clinically indicated. Hypophysitis occurred in 2.5%
(9/355) of patients receiving Opdualag, including Grade 3 (0.3%)
and Grade 2 (1.4%) adverse reactions. Hypophysitis led to permanent
discontinuation of Opdualag in 0.3% and withholding of Opdualag in
0.6% of patients.
Thyroiditis can present with or without endocrinopathy.
Hypothyroidism can follow hyperthyroidism; initiate hormone
replacement or medical management as clinically indicated.
Thyroiditis occurred in 2.8% (10/355) of patients receiving
Opdualag, including Grade 2 (1.1%) adverse reactions. Thyroiditis
did not lead to permanent discontinuation of Opdualag. Thyroiditis
led to withholding of Opdualag in 0.3% of patients. Hyperthyroidism
occurred in 6% (22/355) of patients receiving Opdualag, including
Grade 2 (1.4%) adverse reactions. Hyperthyroidism did not lead to
permanent discontinuation of Opdualag. Hyperthyroidism led to
withholding of Opdualag in 0.3% of patients. Hypothyroidism
occurred in 17% (59/355) of patients receiving Opdualag, including
Grade 2 (11%) adverse reactions. Hypothyroidism led to the
permanent discontinuation of Opdualag in 0.3% and withholding of
Opdualag in 2.5% of patients.
Monitor patients for hyperglycemia or other signs and symptoms
of diabetes; initiate treatment with insulin as clinically
indicated. Diabetes occurred in 0.3% (1/355) of patients receiving
Opdualag, a Grade 3 (0.3%) adverse reaction, and no cases of
diabetic ketoacidosis. Diabetes did not lead to the permanent
discontinuation or withholding of Opdualag in any patient.
Immune-Mediated Nephritis with Renal
Dysfunction
Opdualag can cause immune-mediated nephritis, which is defined
as requiring use of steroids and no clear etiology. In patients
receiving Opdualag, immune-mediated nephritis and renal dysfunction
occurred in 2% (7/355) of patients, including Grade 3 (1.1%) and
Grade 2 (0.8%) adverse reactions. Immune-mediated nephritis and
renal dysfunction led to permanent discontinuation of Opdualag in
0.8% and withholding of Opdualag in 0.6% of patients.
Withhold or permanently discontinue Opdualag depending on
severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information).
Immune-Mediated Dermatologic Adverse
Reactions
Opdualag can cause immune-mediated rash or dermatitis, defined
as requiring use of steroids and no clear alternate etiology.
Exfoliative dermatitis, including Stevens-Johnson syndrome, toxic
epidermal necrolysis, and Drug Rash with eosinophilia and systemic
symptoms has occurred with PD-1/L-1 blocking antibodies. Topical
emollients and/or topical corticosteroids may be adequate to treat
mild to moderate non-exfoliative rashes.
Withhold or permanently discontinue Opdualag depending on
severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information).
Immune-mediated rash occurred in 9% (33/355) of patients,
including Grade 3 (0.6%) and Grade 2 (3.4%) adverse reactions.
Immune-mediated rash did not lead to permanent discontinuation of
Opdualag. Immune- mediated rash led to withholding of Opdualag in
1.4% of patients.
Immune-Mediated Myocarditis
Opdualag can cause immune-mediated myocarditis, which is defined
as requiring use of steroids and no clear alternate etiology. The
diagnosis of immune-mediated myocarditis requires a high index of
suspicion. Patients with cardiac or cardio-pulmonary symptoms
should be assessed for potential myocarditis. If myocarditis is
suspected, withhold dose, promptly initiate high dose steroids
(prednisone or methylprednisolone 1 to 2 mg/kg/day) and promptly
arrange cardiology consultation with diagnostic workup. If
clinically confirmed, permanently discontinue Opdualag for Grade
2-4 myocarditis.
Myocarditis occurred in 1.7% (6/355) of patients receiving
Opdualag, including Grade 3 (0.6%), and Grade 2 (1.1%) adverse
reactions. Myocarditis led to permanent discontinuation of Opdualag
in 1.7% of patients.
Other Immune-Mediated Adverse
Reactions
The following clinically significant IMARs occurred at an
incidence of <1% (unless otherwise noted) in patients who
received Opdualag or were reported with the use of other PD-1/PD-L1
blocking antibodies. Severe or fatal cases have been reported for
some of these adverse reactions: Cardiac/Vascular: pericarditis,
vasculitis; Nervous System: meningitis, encephalitis, myelitis and
demyelination, myasthenic syndrome/myasthenia gravis (including
exacerbation), Guillain-Barré syndrome, nerve paresis, autoimmune
neuropathy; Ocular: uveitis, iritis, and other ocular inflammatory
toxicities can occur. Some cases can be associated with retinal
detachment. Various grades of visual impairment, including
blindness, can occur. If uveitis occurs in combination with other
IMARs, consider a Vogt-Koyanagi-Harada-like syndrome, as this may
require treatment with systemic steroids to reduce the risk of
permanent vision loss; Gastrointestinal: pancreatitis including
increases in serum amylase and lipase levels, gastritis,
duodenitis; Musculoskeletal and Connective Tissue:
myositis/polymyositis, rhabdomyolysis (and associated sequelae
including renal failure), arthritis, polymyalgia rheumatica;
Endocrine: hypoparathyroidism; Other (Hematologic/Immune):
hemolytic anemia, aplastic anemia, hemophagocytic
lymphohistiocytosis, systemic inflammatory response syndrome,
histiocytic necrotizing lymphadenitis (Kikuchi lymphadenitis),
sarcoidosis, immune thrombocytopenic purpura, solid organ
transplant rejection, other transplant (including corneal graft)
rejection.
Infusion-Related Reactions
Opdualag can cause severe infusion-related reactions.
Discontinue Opdualag in patients with severe or life- threatening
infusion-related reactions. Interrupt or slow the rate of infusion
in patients with mild to moderate infusion-related reactions. In
patients who received Opdualag as a 60-minute intravenous infusion,
infusion- related reactions occurred in 7% (23/355) of
patients.
Complications of Allogeneic Hematopoietic Stem Cell
Transplantation (HSCT)
Fatal and other serious complications can occur in patients who
receive allogeneic hematopoietic stem cell transplantation (HSCT)
before or after being treated with a PD-1/PD-L1 receptor blocking
antibody. Transplant- related complications include hyperacute
graft-versus-host disease (GVHD), acute GVHD, chronic GVHD, hepatic
veno-occlusive disease after reduced intensity conditioning, and
steroid-requiring febrile syndrome (without an identified
infectious cause). These complications may occur despite
intervening therapy between PD-1/PD-L1 blockade and allogeneic
HSCT.
Follow patients closely for evidence of transplant-related
complications and intervene promptly. Consider the benefit versus
risks of treatment with a PD-1/PD-L1 receptor blocking antibody
prior to or after an allogeneic HSCT.
Embryo-Fetal Toxicity
Based on its mechanism of action and data from animal studies,
Opdualag can cause fetal harm when administered to a pregnant
woman. Advise pregnant women of the potential risk to a fetus.
Advise females of reproductive potential to use effective
contraception during treatment with Opdualag and for at least 5
months after the last dose of Opdualag.
Lactation
There are no data on the presence of Opdualag in human milk, the
effects on the breastfed child, or the effect on milk production.
Because nivolumab and relatlimab may be excreted in human milk and
because of the potential for serious adverse reactions in a
breastfed child, advise patients not to breastfeed during treatment
with Opdualag and for at least 5 months after the last dose.
Serious Adverse Reactions
In Relativity-047, fatal adverse reactions occurred in 3 (0.8%)
patients who were treated with Opdualag; these included
hemophagocytic lymphohistiocytosis, acute edema of the lung, and
pneumonitis. Serious adverse reactions occurred in 36% of patients
treated with Opdualag. The most frequent serious adverse reactions
reported in ≥1% of patients treated with Opdualag were adrenal
insufficiency (1.4%), anemia (1.4%), colitis (1.4%), pneumonia
(1.4%), acute myocardial infarction (1.1%), back pain (1.1%),
diarrhea (1.1%), myocarditis (1.1%), and pneumonitis (1.1%).
Common Adverse Reactions and Laboratory Abnormalities
The most common adverse reactions reported in ≥20% of the
patients treated with Opdualag were musculoskeletal pain (45%),
fatigue (39%), rash (28%), pruritus (25%), and diarrhea (24%).
The most common laboratory abnormalities that occurred in ≥20%
of patients treated with Opdualag were decreased hemoglobin (37%),
decreased lymphocytes (32%), increased AST (30%), increased ALT
(26%), and decreased sodium (24%).
Please see U.S. Full Prescribing Information for Opdualag.
KRAZATI
INDICATION
KRAZATI is indicated for the treatment of adult patients with
KRASG12C-mutated locally advanced or metastatic non-small cell lung
cancer (NSCLC), as determined by an FDA-approved test, who have
received at least one prior systemic therapy.
This indication is approved under accelerated approval based on
objective response rate (ORR) and duration of response (DOR).
Continued approval for this indication may be contingent upon
verification and description of a clinical benefit in a
confirmatory trial(s).
IMPORTANT SAFETY
INFORMATION
GASTROINTESTINAL ADVERSE REACTIONS
- In the pooled safety population, serious gastrointestinal
adverse reactions observed were gastrointestinal obstruction in
1.6%, including 1.4% grade 3 or 4, gastrointestinal bleeding in
0.5% of patients, including 0.5% grade 3, and colitis in 0.3%,
including 0.3% grade 3. In addition, nausea, diarrhea, or vomiting
occurred in 89% of 366 patients, including 9% grade 3. Nausea,
diarrhea, or vomiting led to dosage interruption or dose reduction
in 29% of patients and permanent discontinuation of KRAZATI in
0.3%
- Monitor and manage patients using supportive care, including
antidiarrheals, antiemetics, or fluid replacement, as indicated.
Withhold, reduce the dose, or permanently discontinue KRAZATI based
on severity
QTC INTERVAL PROLONGATION
- KRAZATI can cause QTc interval prolongation, which can increase
the risk for ventricular tachyarrhythmias (e.g., torsades de
pointes) or sudden death
- In the pooled safety population, 6% of 366 patients with at
least one post-baseline electrocardiogram (ECG) assessment had an
average QTc ≥501 ms, and 11% of patients had an increase from
baseline of QTc >60 msec. KRAZATI causes concentration-dependent
increases in the QTc interval
- Avoid concomitant use of KRAZATI with other products with a
known potential to prolong the QTc interval. Avoid use of KRAZATI
in patients with congenital long QT syndrome and in patients with
concurrent QTc prolongation
- Monitor ECGs and electrolytes prior to starting KRAZATI, during
concomitant use, and as clinically indicated in patients with
congestive heart failure, bradyarrhythmias, electrolyte
abnormalities, and in patients who are taking medications that are
known to prolong the QT interval. Withhold, reduce the dose, or
permanently discontinue KRAZATI, depending on severity
HEPATOTOXICITY
- KRAZATI can cause hepatotoxicity
- In the pooled safety population, hepatotoxicity occurred in
37%, and 7% were grade 3 or 4. A total of 32% of patients who
received KRAZATI had increased alanine aminotransferase
(ALT)/increased aspartate aminotransferase (AST); 5% were grade 3
and 0.5% were grade 4. Increased ALT/AST leading to dose
interruption or reduction occurred in 11% of patients. KRAZATI was
discontinued due to increased ALT/AST in 0.5% of patients
- Monitor liver laboratory tests (AST, ALT, alkaline phosphatase,
and total bilirubin) prior to the start of KRAZATI, and monthly for
3 months or as clinically indicated, with more frequent testing in
patients who develop transaminase elevations. Reduce the dose,
withhold, or permanently discontinue KRAZATI based on severity
INTERSTITIAL LUNG DISEASE /PNEUMONITIS
- KRAZATI can cause interstitial lung disease (ILD)/pneumonitis,
which can be fatal. In the pooled safety population,
ILD/pneumonitis occurred in 4.1% of patients, 1.4% were grade 3 or
4, and 1 case was fatal. The median time to first onset for
ILD/pneumonitis was 12 weeks (range: 5 to 31 weeks). KRAZATI was
discontinued due to ILD/pneumonitis in 0.8% of patients
- Monitor patients for new or worsening respiratory symptoms
indicative of ILD/pneumonitis (eg, dyspnea, cough, fever). Withhold
KRAZATI in patients with suspected ILD/pneumonitis and permanently
discontinue KRAZATI if no other potential causes of ILD/pneumonitis
are identified
ADVERSE REACTIONS
- The most common adverse reactions (≥25%) are nausea, diarrhea,
vomiting, fatigue, musculoskeletal pain, hepatotoxicity, renal
impairment, edema, dyspnea, decreased appetite
FEMALES AND MALES OF REPRODUCTIVE POTENTIAL
- Infertility: Based on findings from animal studies, KRAZATI may
impair fertility in females and males of reproductive
potential
Please see U.S. Full Prescribing Information for
KRAZATI.
BREYANZI
INDICATION
BREYANZI is a CD19-directed genetically modified autologous T
cell immunotherapy indicated for the treatment of:
- adult patients with large B-cell lymphoma (LBCL), including
diffuse large B-cell lymphoma (DLBCL) not otherwise specified
(including DLBCL arising from indolent lymphoma), high-grade B-cell
lymphoma, primary mediastinal large B-cell lymphoma, and follicular
lymphoma grade 3B, who have:
- refractory disease to first-line chemoimmunotherapy or relapse
within 12 months of first-line chemoimmunotherapy; or
- refractory disease to first-line chemoimmunotherapy or relapse
after first line chemoimmunotherapy and are not eligible for
hematopoietic stem cell transplantation (HSCT) due to comorbidities
or age; or
- relapsed or refractory disease after two or more lines of
systemic therapy.
Limitations of Use: BREYANZI is not
indicated for the treatment of patients with primary central
nervous system lymphoma.
- Adult patients with relapsed or refractory chronic lymphocytic
leukemia (CLL) or small lymphocytic lymphoma (SLL) who have
received at least 2 prior lines of therapy, including a Bruton
tyrosine kinase (BTK) inhibitor and a B-cell lymphoma 2 (BCL-2)
inhibitor. This indication is approved under accelerated approval
based on response rate and duration of response. Continued approval
for this indication may be contingent upon verification and
description of clinical benefit in confirmatory trial(s).
- Adult patients with relapsed or refractory follicular lymphoma
(FL) who have received 2 or more prior lines of systemic therapy.
This indication is approved under accelerated approval based on
response rate and duration of response. Continued approval for this
indication may be contingent upon verification and description of
clinical benefit in confirmatory trial(s).
Important Safety
Information
WARNING: CYTOKINE RELEASE SYNDROME,
NEUROLOGIC TOXICITIES, AND SECONDARY HEMATOLOGICAL
MALIGNANCIES
- Cytokine Release Syndrome (CRS), including fatal or
life-threatening reactions, occurred in patients receiving
BREYANZI. Do not administer BREYANZI to patients with active
infection or inflammatory disorders. Treat severe or
life-threatening CRS with tocilizumab with or without
corticosteroids.
- Neurologic toxicities, including fatal or life-threatening
reactions, occurred in patients receiving BREYANZI, including
concurrently with CRS, after CRS resolution, or in the absence of
CRS. Monitor for neurologic events after treatment with BREYANZI.
Provide supportive care and/or corticosteroids as needed
- T cell malignancies have occurred following treatment of
hematologic malignancies with BCMA- and CD19-directed genetically
modified autologous T cell immunotherapies, including
BREYANZI
- BREYANZI is available only through a restricted program
under a Risk Evaluation and Mitigation Strategy (REMS) called the
BREYANZI REMS.
Cytokine Release Syndrome (CRS)
Cytokine release syndrome (CRS), including fatal or
life-threatening reactions, occurred following treatment with
BREYANZI. In clinical trials of BREYANZI which enrolled a total of
614 patients with non-Hodgkin lymphoma (NHL), CRS occurred in 53%
of patients, including Grade 3 or higher CRS in 4% of patients. The
median time to onset was 5 days (range: 1 to 63 days). CRS resolved
in 98% of patients with median duration of 5 days (range: 1 to 37
days). The most common manifestations of CRS (>10%) were fever, hypotension, tachycardia,
chills, hypoxia and headache.
Serious events that may be associated with CRS include cardiac
arrhythmias (including atrial fibrillation and ventricular
tachycardia), cardiac arrest, cardiac failure, diffuse alveolar
damage, renal insufficiency, capillary leak syndrome, hypotension,
hypoxia, and hemophagocytic lymphohistiocytosis/macrophage
activation syndrome (HLH/MAS).
Ensure that 2 doses of tocilizumab are available prior to
infusion of BREYANZI.
Neurologic Toxicities
Neurologic toxicities that were fatal or life-threatening,
including immune effector cell-associated neurotoxicity syndrome
(ICANS), occurred following treatment with BREYANZI. Serious events
including cerebral edema and seizures occurred with BREYANZI. Fatal
and serious cases of leukoencephalopathy, some attributable to
fludarabine, also occurred.
In clinical trials of BREYANZI, CAR T cell-associated neurologic
toxicities occurred in 31% of patients, including > Grade 3 cases in 10% of patients. The median
time to onset of neurotoxicity was 8 days (range: 1 to 63 days).
Neurologic toxicities resolved in 87% of patients with a median
duration of 8 days (range: 1 to 119 days). Of patients developing
neurotoxicity, 81% also developed CRS.
The most common neurologic toxicities (≥ 5%) included
encephalopathy, tremor, aphasia, headache, dizziness, and
delirium.
CRS and Neurologic Toxicities Monitoring
Monitor patients daily for at least 7 days following BREYANZI
infusion at a REMS-certified healthcare facility for signs and
symptoms of CRS and neurologic toxicities and assess for other
causes of neurological symptoms. Monitor patients for signs and
symptoms of CRS and neurologic toxicities for at least 4 weeks
after infusion and treat promptly. At the first sign of CRS,
institute treatment with supportive care, tocilizumab, or
tocilizumab and corticosteroids as indicated. Manage neurologic
toxicity with supportive care and/or corticosteroid as needed.
Counsel patients to seek immediate medical attention should signs
or symptoms of CRS or neurologic toxicity occur at any time.
BREYANZI REMS
Because of the risk of CRS and neurologic toxicities, BREYANZI
is available only through a restricted program under a Risk
Evaluation and Mitigation Strategy (REMS) called the BREYANZI REMS.
The required components of the BREYANZI REMS are:
- Healthcare facilities that dispense and administer BREYANZI
must be enrolled and comply with the REMS requirements.
- Certified healthcare facilities must have on-site, immediate
access to tocilizumab.
- Ensure that a minimum of 2 doses of tocilizumab are available
for each patient for infusion within 2 hours after BREYANZI
infusion, if needed for treatment of CRS.
Further information is available at www.BreyanziREMS.com, or
contact Bristol Myers Squibb at 1-866-340-7332.
Hypersensitivity Reactions
Allergic reactions may occur with the infusion of BREYANZI.
Serious hypersensitivity reactions, including anaphylaxis, may be
due to dimethyl sulfoxide (DMSO).
Serious Infections
Severe infections, including life-threatening or fatal
infections, have occurred in patients after BREYANZI infusion. In
clinical trials of BREYANZI, infections of any grade occurred in
33% of patients, with Grade 3 or higher infections occurring in 12%
of all patients. Grade 3 or higher infections with an unspecified
pathogen occurred in 7%, bacterial infections in 4%, viral
infections in 2%, and fungal infections in 0.7% of patients. One
patient who received four prior lines of therapy developed a fatal
case of John Cunningham (JC) virus progressive multifocal
leukoencephalopathy four months after treatment with BREYANZI.
Febrile neutropenia developed after BREYANZI infusion in 8% of
patients. Febrile neutropenia may be concurrent with CRS. In the
event of febrile neutropenia, evaluate for infection and manage
with broad spectrum antibiotics, fluids, and other supportive care
as medically indicated.
Monitor patients for signs and symptoms of infection before and
after BREYANZI administration and treat appropriately. Administer
prophylactic antimicrobials according to standard institutional
guidelines. Avoid administration of BREYANZI in patients with
clinically significant, active systemic infections.
Viral reactivation: Hepatitis B virus (HBV) reactivation, in
some cases resulting in fulminant hepatitis, hepatic failure, and
death, can occur in patients treated with drugs directed against B
cells. In clinical trials of BREYANZI, 26 of 29 patients with prior
history of HBV were treated with concurrent antiviral suppressive
therapy. Perform screening for HBV, HCV, and HIV in accordance with
clinical guidelines before collection of cells for manufacturing.
In patients with prior history of HBV, consider concurrent
antiviral suppressive therapy to prevent HBV reactivation per
standard guidelines.
Prolonged Cytopenias
Patients may exhibit cytopenias not resolved for several weeks
following lymphodepleting chemotherapy and BREYANZI infusion. In
clinical trials of BREYANZI, Grade 3 or higher cytopenias persisted
at Day 29 following BREYANZI infusion in 34% of patients, and
included thrombocytopenia in 24%, neutropenia in 22%, and anemia in
7% of patients. Monitor complete blood counts prior to and after
BREYANZI administration.
Hypogammaglobulinemia
B-cell aplasia and hypogammaglobulinemia can occur in patients
receiving treatment with BREYANZI. In clinical trials of BREYANZI,
hypogammaglobulinemia was reported as an adverse reaction in 10% of
patients. Hypogammaglobulinemia, either as an adverse reaction or
laboratory IgG level below 500 mg/dL after infusion, was reported
in 29% of patients. Monitor immunoglobulin levels after treatment
with BREYANZI and manage using infection precautions, antibiotic
prophylaxis, and immunoglobulin replacement as clinically
indicated.
Live vaccines: The safety of immunization with live viral
vaccines during or following BREYANZI treatment has not been
studied. Vaccination with live virus vaccines is not recommended
for at least 6 weeks prior to the start of lymphodepleting
chemotherapy, during BREYANZI treatment, and until immune recovery
following treatment with BREYANZI.
Secondary Malignancies
Patients treated with BREYANZI may develop secondary
malignancies. T cell malignancies have occurred following treatment
of hematologic malignancies with BCMA- and CD19-directed
genetically modified autologous T cell immunotherapies, including
BREYANZI. Mature T cell malignancies, including CAR-positive
tumors, may present as soon as weeks following infusion, and may
include fatal outcomes. Monitor lifelong for secondary
malignancies. In the event that a secondary malignancy occurs,
contact Bristol Myers Squibb at 1-888-805-4555 for reporting and to
obtain instructions on collection of patient samples for
testing.
Effects on Ability to Drive and Use Machines
Due to the potential for neurologic events, including altered
mental status or seizures, patients receiving BREYANZI are at risk
for developing altered or decreased consciousness or impaired
coordination in the 8 weeks following BREYANZI administration.
Advise patients to refrain from driving and engaging in hazardous
occupations or activities, such as operating heavy or potentially
dangerous machinery, for at least 8 weeks.
Immune Effector Cell-Associated Hemophagocytic
Lymphohistiocytosis-Like Syndrome (IEC-HS)
Immune Effector Cell-Associated Hemophagocytic
Lymphohistiocytosis (IEC-HS), including fatal or life-threatening
reactions, occurred following treatment with BREYANZI. Three of 89
(3%) safety evaluable patients with R/R CLL/SLL developed IEC-HS.
Time to onset of IEC-HS ranged from 7 to 18 days. Two of the 3
patients developed IEC-HS in the setting of ongoing CRS and 1 in
the setting of ongoing neurotoxicity. IEC-HS was fatal in 2 of 3
patients. One patient had fatal IEC-HS and one had ongoing IEC-HS
at time of death. IEC-HS is a life-threatening condition with a
high mortality rate if not recognized and treated early. Treatment
of IEC-HS should be administered per current practice
guidelines.
Adverse Reactions
The most common adverse reactions (incidence ≥ 30%) in:
- LBCL are fever, cytokine release syndrome, fatigue,
musculoskeletal pain, and nausea. The most common Grade 3-4
laboratory abnormalities include lymphocyte count decrease,
neutrophil count decrease, platelet count decrease, and hemoglobin
decrease.
- CLL/SLL are cytokine release syndrome, encephalopathy, fatigue,
musculoskeletal pain, nausea, edema, and diarrhea. The most common
Grade 3-4 laboratory abnormalities include neutrophil count
decrease, white blood cell decrease, hemoglobin decrease, platelet
count decrease, and lymphocyte count decrease.
- FL are cytokine release syndrome. The most common Grade 3-4
laboratory abnormalities include lymphocyte count decreased,
neutrophil count decreased, and white blood cell decrease.
Please see full Prescribing Information, including Boxed
WARNINGS and Medication Guide.
REBLOZYL
REBLOZYL® (luspatercept-aamt) is indicated for the treatment of
anemia without previous erythropoiesis stimulating agent use
(ESA-naïve) in adult patients with very low- to intermediate-risk
myelodysplastic syndromes (MDS) who may require regular red blood
cell (RBC) transfusions.
REBLOZYL® (luspatercept-aamt) is indicated for the treatment of
anemia failing an erythropoiesis stimulating agent and requiring 2
or more red blood cell (RBC) units over 8 weeks in adult patients
with very low- to intermediate-risk myelodysplastic syndromes with
ring sideroblasts (MDS-RS) or with
myelodysplastic/myeloproliferative neoplasm with ring sideroblasts
and thrombocytosis (MDS/MPN-RS-T).
REBLOZYL is not indicated for use as a substitute for RBC
transfusions in patients who require immediate correction of
anemia.
Important Safety
Information
WARNINGS AND PRECAUTIONS
Thrombosis/Thromboembolism
In adult patients with beta thalassemia, thromboembolic events
(TEE) were reported in 8/223 (3.6%) of REBLOZYL-treated patients.
TEEs included deep vein thrombosis, pulmonary embolus, portal vein
thrombosis, and ischemic stroke. Patients with known risk factors
for thromboembolism (splenectomy or concomitant use of hormone
replacement therapy) may be at further increased risk of
thromboembolic conditions. Consider thromboprophylaxis in patients
at increased risk of TEE. Monitor patients for signs and symptoms
of thromboembolic events and institute treatment promptly.
Hypertension
Hypertension was reported in 11.4% (63/554) of REBLOZYL-treated
patients. Across clinical studies, the incidence of Grade 3 to 4
hypertension ranged from 2% to 9.6%. In ESA-refractory or
-intolerant adult patients with MDS with normal baseline blood
pressure, 26 (30%) patients developed systolic blood pressure (SBP)
≥130 mm Hg and 23 (16%) patients developed diastolic blood pressure
(DBP) ≥80 mm Hg. In ESA-naïve adult patients with MDS with normal
baseline blood pressure, 23 (36%) patients developed SBP ≥140 mm Hg
and 11 (6%) patients developed DBP ≥80 mm Hg. Monitor blood
pressure prior to each administration. Manage new or exacerbations
of preexisting hypertension using anti-hypertensive agents.
Embryo-Fetal Toxicity
REBLOZYL may cause fetal harm when administered to a pregnant
woman. REBLOZYL caused increased post-implantation loss, decreased
litter size, and an increased incidence of skeletal variations in
pregnant rat and rabbit studies. Advise pregnant women of the
potential risk to a fetus. Advise females of reproductive potential
to use effective contraception during treatment and for at least 3
months after the final dose.
ADVERSE REACTIONS
ESA-naïve adult patients with Myelodysplastic
Syndromes
Grade ≥3 (≥2%) adverse reactions included hypertension and
dyspnea.
The most common (≥10%) all-grade adverse reactions included
diarrhea, fatigue, hypertension, peripheral edema, nausea, and
dyspnea.
ESA-refractory or -intolerant adult patients with
Myelodysplastic Syndromes
Grade ≥3 (≥2%) adverse reactions included fatigue, hypertension,
syncope and musculoskeletal pain. A fatal adverse reaction occurred
in 5 (2.1%) patients.
The most common (≥10%) adverse reactions included fatigue,
musculoskeletal pain, dizziness, diarrhea, nausea, hypersensitivity
reactions, hypertension, headache, upper respiratory tract
infection, bronchitis, and urinary tract infection.
LACTATION
It is not known whether REBLOZYL is excreted into human milk or
absorbed systemically after ingestion by a nursing infant. REBLOZYL
was detected in milk of lactating rats. When a drug is present in
animal milk, it is likely that the drug will be present in human
milk. Because many drugs are excreted in human milk, and because of
the unknown effects of REBLOZYL in infants, a decision should be
made whether to discontinue nursing or to discontinue treatment.
Because of the potential for serious adverse reactions in the
breastfed child, breastfeeding is not recommended during treatment
and for 3 months after the last dose.
DRUG ABUSE POTENTIAL
Abuse: Abuse of REBLOZYL may be seen in athletes for the effects
on erythropoiesis. Misuse of drugs that increase erythropoiesis,
such as REBLOZYL, by healthy persons may lead to polycythemia,
which may be associated with life-threatening cardiovascular
complications.
Please see U.S. Full Prescribing Information for REBLOZYL.
ABECMA
INDICATION
ABECMA (idecabtagene vicleucel) is a B-cell maturation antigen
(BCMA)-directed genetically modified autologous T cell
immunotherapy indicated for the treatment of adult patients with
relapsed or refractory multiple myeloma after two or more prior
lines of therapy, including an immunomodulatory agent, a proteasome
inhibitor, and an anti-CD38 monoclonal antibody.
IMPORTANT SAFETY
INFORMATION
WARNING: CYTOKINE RELEASE SYNDROME,
NEUROLOGIC TOXICITIES, HLH/MAS, PROLONGED CYTOPENIA and SECONDARY
HEMATOLOGICAL MALIGNANCIES
- Cytokine Release Syndrome (CRS),
including fatal or life-threatening reactions, occurred in patients
following treatment with ABECMA. Do not administer ABECMA to
patients with active infection or inflammatory disorders. Treat
severe or life-threatening CRS with tocilizumab or tocilizumab and
corticosteroids.
- Neurologic Toxicities, which may be
severe or life-threatening, occurred following treatment with
ABECMA, including concurrently with CRS, after CRS resolution, or
in the absence of CRS. Monitor for neurologic events after
treatment with ABECMA. Provide supportive care and/or
corticosteroids as needed. Hemophagocytic
Lymphohistiocytosis/Macrophage Activation Syndrome (HLH/MAS)
including fatal and life-threatening reactions, occurred in
patients following treatment with ABECMA. HLH/MAS can occur with
CRS or neurologic toxicities. Prolonged Cytopenia with bleeding and
infection, including fatal outcomes following stem cell
transplantation for hematopoietic recovery, occurred following
treatment with ABECMA.
- T cell malignancies have occurred
following treatment of hematologic malignancies with BCMA- and
CD19-directed genetically modified autologous T cell
immunotherapies, including ABECMA.
- ABECMA is available only through a
restricted program under a Risk Evaluation and Mitigation Strategy
(REMS) called the ABECMA REMS.
Warnings and Precautions:
Early Death:
In KarMMa-3, a randomized (2:1), controlled trial, a higher
proportion of patients experienced death within 9 months after
randomization in the ABECMA arm (45/254; 18%) compared to the
standard regimens arm (15/132; 11%). Early deaths occurred in 8%
(20/254) and 0% prior to ABECMA infusion and standard regimen
administration, respectively, and 10% (25/254) and 11% (15/132)
after ABECMA infusion and standard regimen administration,
respectively. Out of the 20 deaths that occurred prior to ABECMA
infusion, 15 occurred from disease progression, 3 occurred from
adverse events and 2 occurred from unknown causes. Out of the 25
deaths that occurred after ABECMA infusion, 10 occurred from
disease progression, 11 occurred from adverse events, and 4
occurred from unknown causes.
Cytokine Release Syndrome (CRS): CRS, including fatal or
life-threatening reactions, occurred following treatment with
ABECMA. Among patients receiving ABECMA for relapsed refractory
multiple myeloma in the KarMMa and KarMMa-3 studies (N=349), CRS
occurred in 89% (310/349), including ≥ Grade 3 CRS (Lee grading
system) in 7% (23/349) of patients and Grade 5 CRS in 0.9% (3/349)
of patients. The median time-to-onset of CRS, any grade, was 1 day
(range: 1 to 27 days), and the median duration of CRS was 5 days
(range: 1 to 63 days). In the pooled studies, the rate of ≥Grade 3
CRS was 10% (7/71) for patients treated in dose range of 460 to 510
x 106 CAR-positive T cells and 5.4% (13/241) for patients treated
in dose range of 300 to 460 x 106 CAR-positive T cells. The most
common manifestations of CRS (greater than or equal to 10%)
included pyrexia (87%), hypotension (30%), tachycardia (26%),
chills (19%), hypoxia (16%). Grade 3 or higher events that may be
associated with CRS include hypotension, hypoxia,
hyperbilirubinemia, hypofibrinogenemia, ARDS, atrial fibrillation,
hepatocellular injury, metabolic acidosis, pulmonary edema,
coagulopathy, renal failure, multiple organ dysfunction syndrome
and HLH/MAS.
Identify CRS based on clinical presentation. Evaluate for and
treat other causes of fever, hypoxia, and hypotension. CRS has been
reported to be associated with findings of HLH/MAS, and the
physiology of the syndromes may overlap. HLH/MAS is a potentially
life-threatening condition. In patients with progressive symptoms
of CRS or refractory CRS despite treatment, evaluate for evidence
of HLH/MAS.
Of the 349 patients who received ABECMA in clinical trials, 226
(65%) patients received tocilizumab; 39% (135/349) received a
single dose, while 26% (91/349) received more than 1 dose of
tocilizumab. Overall, 24% (82/349) of patients received at least 1
dose of corticosteroids for treatment of CRS. Almost all patients
who received corticosteroids for CRS also received tocilizumab. For
patients treated in dose range of 460 to 510 x 106 CAR-positive T
cells, 76% (54/71) of patients received tocilizumab and 35% (25/71)
received at least 1 dose of corticosteroids for treatment of CRS.
For patients treated in dose range of 300 to 460 x 106 CAR-positive
T cells, 63% (152/241) of patients received tocilizumab and 20%
(49/241) received at least 1 dose of corticosteroid for treatment
of CRS.
Monitor patients at least daily for 7 days following ABECMA
infusion at the REMS-certified healthcare facility for signs or
symptoms of CRS and monitor patients for signs or symptoms of CRS
for at least 4 weeks after ABECMA infusion. At the first sign of
CRS, institute treatment with supportive care, tocilizumab and/or
corticosteroids as indicated. Ensure that a minimum of 2 doses of
tocilizumab are available prior to infusion of ABECMA.
Counsel patients to seek immediate medical attention should
signs or symptoms of CRS occur at any time.
Neurologic Toxicities: Neurologic toxicities, including
immune-effector cell-associated neurotoxicity (ICANS), which may be
severe or life-threatening, occurred concurrently with CRS, after
CRS resolution, or in the absence of CRS following treatment with
ABECMA. In patients receiving ABECMA in the KarMMa and KarMMa-3
studies, CAR T cell-associated neurotoxicity occurred in 40%
(139/349), including Grade 3 in 4% (14/349) and Grade 4 in 0.6%
(2/349) of patients. The median time to onset of neurotoxicity was
2 days (range: 1 to 148 days). The median duration of CAR T
cell-associated neurotoxicity was 8 days (range: 1 to 720 days) in
all patients including those with ongoing neurologic events at the
time of death or data cut off. CAR T cell-associated neurotoxicity
resolved in 123 of 139 (88%) patients and median time to resolution
was 5 days (range: 1 to 245 days). One-hundred and thirty four out
of 349 (38%) patients with neurotoxicity had CRS. The onset of
neurotoxicity during CRS was observed in 93 patients, before the
onset of CRS in 12 patients, and after the CRS event in 29
patients. The rate of Grade 3 or 4 CAR T cell-associated
neurotoxicity was 5.6% (4/71) and 3.7% (9/241) for patients treated
in dose range of 460 to 510 x 106 CAR-positive T cells and 300 to
460 x 106 CAR-positive T cells, respectively. The most frequent
(greater than or equal to 5%) manifestations of CAR T
cell-associated neurotoxicity include encephalopathy (21%),
headache (15%), dizziness (8%), delirium (6%), and tremor (6%).
At the safety update for KarMMa-3 study, one patient developed
fatal neurotoxicity 43 days after ABECMA. In KarMMa, one patient
had ongoing Grade 2 neurotoxicity at the time of death. Two
patients had ongoing Grade 1 tremor at the time of data cutoff.
Cerebral edema has been associated with ABECMA in a patient in
another study in multiple myeloma. Grade 3 myelitis and Grade 3
parkinsonism have occurred after treatment with ABECMA in another
study in multiple myeloma.
Monitor patients at least daily for 7 days following ABECMA
infusion at the REMS-certified healthcare facility for signs or
symptoms of neurologic toxicities and monitor patients for signs or
symptoms of neurologic toxicities for at least 4 weeks after ABECMA
infusion and treat promptly. Rule out other causes of neurologic
symptoms. Neurologic toxicity should be managed with supportive
care and/or corticosteroids as needed. Counsel patients to seek
immediate medical attention should signs or symptoms occur at any
time.
Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage
Activation Syndrome (MAS): In patients receiving ABECMA in the
KarMMa and KarMMa-3 studies, HLH/MAS occurred in 2.9% (10/349) of
patients. All events of HLH/MAS had onset within 10 days of
receiving ABECMA, with a median onset of 6.5 days (range: 4 to 10
days) and occurred in the setting of ongoing or worsening CRS. Five
patients with HLH/MAS had overlapping neurotoxicity. The
manifestations of HLH/MAS include hypotension, hypoxia, multiple
organ dysfunction, renal dysfunction and cytopenia.
In KarMMa-3, one patient had Grade 5, two patients had Grade 4
and two patients had Grade 3 HLH/MAS. The patient with Grade 5
HLH/MAS also had Grade 5 candida sepsis and Grade 5 CRS. In another
patient who died due to stroke, the Grade 4 HLH/MAS had resolved
prior to death. Two cases of Grade 3 and one case of Grade 4
HLH/MAS had resolved.
In KarMMa, one patient treated in the 300 x 106 CAR-positive T
cells dose cohort developed fatal multi-organ HLH/MAS with CRS. In
another patient with fatal bronchopulmonary aspergillosis, HLH/MAS
was contributory to the fatal outcome. Three cases of Grade 2
HLH/MAS resolved.
HLH/MAS is a potentially life-threatening condition with a high
mortality rate if not recognized early and treated. Treatment of
HLH/MAS should be administered per institutional guidelines.
ABECMA REMS: Due to the risk of CRS and neurologic
toxicities, ABECMA is available only through a restricted program
under a Risk Evaluation and Mitigation Strategy (REMS) called the
ABECMA REMS. Further information is available at www.AbecmaREMS.com
or contact Bristol-Myers Squibb at 1-866-340-7332.
Hypersensitivity Reactions: Allergic reactions may occur
with the infusion of ABECMA. Serious hypersensitivity reactions,
including anaphylaxis, may be due to dimethyl sulfoxide (DMSO) in
ABECMA.
Infections: ABECMA should not be administered to patients
with active infections or inflammatory disorders. Severe,
life-threatening, or fatal infections occurred in patients after
ABECMA infusion.
In all patients receiving ABECMA in the KarMMa and KarMMa-3
studies, infections (all grades) occurred in 61% of patients. Grade
3 or 4 infections occurred in 21% of patients. Grade 3 or 4
infections with an unspecified pathogen occurred in 12%, viral
infections in 7%, bacterial infections in 4.3%, and fungal
infections in 1.4% of patients. Overall, 15 patients had Grade 5
infections (4.3%); 8 patients (2.3%) with infections of pathogen
unspecified, 3 patients (0.9%) with fungal infections, 3 patients
(0.9%) with viral infections, and 1 patient (0.3%) with bacterial
infection.
Monitor patients for signs and symptoms of infection before and
after ABECMA infusion and treat appropriately. Administer
prophylactic, pre-emptive, and/or therapeutic antimicrobials
according to standard institutional guidelines.
Febrile neutropenia was observed in 38% (133/349) of patients
after ABECMA infusion and may be concurrent with CRS. In the event
of febrile neutropenia, evaluate for infection and manage with
broad-spectrum antibiotics, fluids, and other supportive care as
medically indicated.
Viral Reactivation: Cytomegalovirus (CMV) infection resulting in
pneumonia and death has occurred following ABECMA administration.
Monitor and treat for CMV reactivation in accordance with clinical
guidelines. Hepatitis B virus (HBV) reactivation, in some cases
resulting in fulminant hepatitis, hepatic failure, and death, can
occur in patients treated with drugs directed against plasma cells.
Perform screening for CMV, HBV, hepatitis C virus (HCV), and human
immunodeficiency virus (HIV) in accordance with clinical guidelines
before collection of cells for manufacturing. Consider antiviral
therapy to prevent viral reactivation per local institutional
guidelines/clinical practice.
Prolonged Cytopenias: In patients receiving ABECMA in the
KarMMa and KarMMa-3 studies, 40% of patients (139/349) experienced
prolonged Grade 3 or 4 neutropenia and 42% (145/349) experienced
prolonged Grade 3 or 4 thrombocytopenia that had not resolved by
Month 1 following ABECMA infusion. In 89% (123/139) of patients who
recovered from Grade 3 or 4 neutropenia after Month 1, the median
time to recovery from ABECMA infusion was 1.9 months. In 76%
(110/145) of patients who recovered from Grade 3 or 4
thrombocytopenia, the median time to recovery was 1.9 months. Five
patients underwent stem cell therapy for hematopoietic
reconstitution due to prolonged cytopenia. The rate of Grade 3 or 4
thrombocytopenia was 62% (44/71) and 56% (135/241) for patients
treated in dose range of 460 to 510 x 106 CAR-positive T cells and
300 to 460 x 106 CAR-positive T cells, respectively.
Monitor blood counts prior to and after ABECMA infusion. Manage
cytopenia with myeloid growth factor and blood product transfusion
support according to local institutional guidelines.
Hypogammaglobulinemia: In all patients receiving ABECMA
in the KarMMa and KarMMa-3 studies, hypogammaglobulinemia was
reported as an adverse event in 13% (46/349) of patients;
laboratory IgG levels fell below 500 mg/dL after infusion in 37%
(130/349) of patients treated with ABECMA.
Hypogammaglobulinemia either as an adverse reaction or
laboratory IgG level below 500 mg/dL after infusion occurred in 45%
(158/349) of patients treated with ABECMA. Forty-one percent of
patients received intravenous immunoglobulin (IVIG) post-ABECMA for
serum IgG <400 mg/dL.
Monitor immunoglobulin levels after treatment with ABECMA and
administer IVIG for IgG <400 mg/dl. Manage appropriately per
local institutional guidelines, including infection precautions and
antibiotic or antiviral prophylaxis.
Use of Live Vaccines: The safety of immunization with live viral
vaccines during or after ABECMA treatment has not been studied.
Vaccination with live virus vaccines is not recommended for at
least 6 weeks prior to the start of lymphodepleting chemotherapy,
during ABECMA treatment, and until immune recovery following
treatment with ABECMA.
Secondary Malignancies: Patients treated with ABECMA may
develop secondary malignancies. In KarMMa-3, myeloid neoplasms
(four cases of myelodysplastic syndrome and one case of acute
myeloid leukemia) occurred in 2.2% (5/222) of patients following
treatment with ABECMA compared to none in the standard regimens arm
at the time of the safety update. The median time to onset of
myeloid neoplasm from ide-cel infusion was 338 days (Range: 277 to
794 days). Three of these five patients have died following the
development of myeloid neoplasm. One out of the five cases of
myeloid neoplasm occurred after initiation of subsequent
antimyeloma therapy.
T cell malignancies have occurred following treatment of
hematologic malignancies with BCMA- and CD19-directed genetically
modified autologous T cell immunotherapies, including ABECMA.
Mature T cell malignancies, including CAR-positive tumors, may
present as soon as weeks following infusion, and may include fatal
outcomes.
Monitor life-long for secondary malignancies. In the event that
a secondary malignancy occurs, contact Bristol-Myers Squibb at
1-888-805-4555 for reporting and to obtain instructions on
collection of patient samples for testing of secondary
malignancy.
Effects on Ability to Drive and Operate Machinery: Due to
the potential for neurologic events, including altered mental
status or seizures, patients receiving ABECMA are at risk for
altered or decreased consciousness or coordination in the 8 weeks
following ABECMA infusion. Advise patients to refrain from driving
and engaging in hazardous occupations or activities, such as
operating heavy or potentially dangerous machinery, during this
initial period.
Adverse Reactions: The most common nonlaboratory adverse
reactions (incidence greater than or equal to 20%) include pyrexia,
CRS, hypogammaglobulinemia, infections - pathogen unspecified,
musculoskeletal pain, fatigue, febrile neutropenia, hypotension,
tachycardia, diarrhea, nausea, headache, chills, upper respiratory
tract infection, encephalopathy, edema, dyspnea and viral
infections.
Please see full Prescribing Information, including Boxed
WARNINGS and Medication Guide.
INREBIC
INDICATION
INREBIC® (fedratinib) is indicated for the treatment of adult
patients with intermediate-2 or high-risk primary or secondary
(post-polycythemia vera or post-essential thrombocythemia)
myelofibrosis (MF).
U.S. IMPORTANT SAFETY
INFORMATION
WARNING: ENCEPHALOPATHY INCLUDING WERNICKE’S
Serious and fatal encephalopathy, including Wernicke’s, has
occurred in patients treated with INREBIC. Wernicke’s
encephalopathy is a neurologic emergency. Assess thiamine levels in
all patients prior to starting INREBIC, periodically during
treatment, and as clinically indicated. Do not start INREBIC in
patients with thiamine deficiency; replete thiamine prior to
treatment initiation. If encephalopathy is suspected, immediately
discontinue INREBIC and initiate parenteral thiamine. Monitor until
symptoms resolve or improve and thiamine levels normalize.
WARNINGS AND PRECAUTIONS
Encephalopathy, including Wernicke’s: Serious and fatal
encephalopathy, including Wernicke’s encephalopathy, has occurred
in INREBIC-treated patients. Serious cases were reported in 1.3%
(8/608) of patients treated with INREBIC in clinical trials and
0.16% (1/608) of cases were fatal.
Wernicke’s encephalopathy is a neurologic emergency resulting
from thiamine (Vitamin B1) deficiency. Signs and symptoms of
Wernicke’s encephalopathy may include ataxia, mental status
changes, and ophthalmoplegia (e.g., nystagmus, diplopia). Any
change in mental status, confusion, or memory impairment should
raise concern for potential encephalopathy, including Wernicke’s,
and prompt a full evaluation including a neurologic examination,
assessment of thiamine levels, and imaging. Assess thiamine levels
in all patients prior to starting INREBIC, periodically during
treatment, and as clinically indicated. Do not start INREBIC in
patients with thiamine deficiency; replete thiamine prior to
treatment initiation. If encephalopathy is suspected, immediately
discontinue INREBIC and initiate parenteral thiamine. Monitor until
symptoms resolve or improve and thiamine levels normalize.
Anemia: New or worsening Grade 3 anemia occurred in 34%
of INREBIC-treated patients. The median time to onset of the first
Grade 3 anemia was approximately 2 months, with 75% of cases
occurring within 3 months. Mean hemoglobin levels reached nadir
after 12 to 16 weeks with partial recovery and stabilization after
16 weeks. Red blood cell transfusions were received by 51% of
INREBIC-treated patients and permanent discontinuation of INREBIC
occurred due to anemia in 1% of patients. Consider dose reduction
for patients who become red blood cell transfusion dependent.
Thrombocytopenia: New or worsening Grade ≥3
thrombocytopenia during the randomized treatment period occurred in
12% of INREBIC-treated patients. The median time to onset of the
first Grade 3 thrombocytopenia was approximately 1 month; with 75%
of cases occurring within 4 months. Platelet transfusions were
received by 3.1% of INREBIC-treated patients. Permanent
discontinuation of treatment due to thrombocytopenia and bleeding
that required clinical intervention both occurred in 2.1% of
INREBIC-treated patients. Obtain a complete blood count (CBC) at
baseline, periodically during treatment, and as clinically
indicated. For Grade 3 thrombocytopenia with active bleeding or
Grade 4 thrombocytopenia, interrupt INREBIC until resolved to less
than or equal to Grade 2 or baseline. Restart dose at 100 mg daily
below the last given dose and monitor platelets as clinically
indicated.
Gastrointestinal Toxicity: Gastrointestinal toxicities
are the most frequent adverse reactions in INREBIC-treated
patients. During the randomized treatment period, diarrhea occurred
in 66% of patients, nausea in 62% of patients, and vomiting in 39%
of patients. Grade 3 diarrhea 5% and vomiting 3.1% occurred. The
median time to onset of any grade nausea, vomiting, and diarrhea
was 1 day, with 75% of cases occurring within 2 weeks of treatment.
Consider providing appropriate prophylactic anti-emetic therapy
(e.g., 5-HT3 receptor antagonists) during INREBIC treatment. Treat
diarrhea with anti-diarrheal medications promptly at the first
onset of symptoms. Grade 3 or higher nausea, vomiting, or diarrhea
not responsive to supportive measures within 48 hours, interrupt
INREBIC until resolved to Grade 1 or less or baseline. Restart dose
at 100 mg daily below the last given dose. Monitor thiamine levels
and replete as needed.
Hepatic Toxicity: Elevations of ALT and AST (all grades)
during the randomized treatment period occurred in 43% and 40%,
respectively, with Grade 3 or 4 in 1% and 0%, respectively, of
INREBIC-treated patients. The median time to onset of any grade
transaminase elevation was approximately 1 month, with 75% of cases
occurring within 3 months. Monitor hepatic function at baseline,
periodically during treatment, and as clinically indicated. For
Grade 3 or higher ALT and/or AST elevations (greater than 5 × ULN),
interrupt INREBIC dose until resolved to Grade 1 or less or to
baseline. Restart dose at 100 mg daily below the last given dose.
If re-occurrence of a Grade 3 or higher elevation of ALT/AST,
discontinue treatment with INREBIC.
Amylase and Lipase Elevation: Grade 3 or higher amylase
2% and/or lipase 10% elevations developed in INREBIC-treated
patients. The median time to onset of any grade amylase or lipase
elevation was 15 days, with 75% of cases occurring within 1 month
of starting treatment. One patient developed pancreatitis in the
fedratinib clinical development program (n=608) and pancreatitis
resolved with treatment discontinuation. Monitor amylase and lipase
at baseline, periodically during treatment, and as clinically
indicated. For Grade 3 or higher amylase and/or lipase elevations,
interrupt INREBIC until resolved to Grade 1 or less or to baseline.
Restart dose at 100 mg daily below the last given dose.
ADVERSE REACTIONS:
The most common adverse reactions for INREBIC treated vs.
placebo were diarrhea (66% vs. 16%), nausea (62% vs. 15%), anemia
(40% vs. 14%), and vomiting (39% vs. 5%). Dosage interruptions due
to an adverse reaction during the randomized treatment period
occurred in 21% of patients who received INREBIC. Adverse reactions
requiring dosage interruption in >3% of patients who received
INREBIC included diarrhea and nausea. Dosage reductions due to an
adverse reaction during the randomized treatment period occurred in
19% of patients who received INREBIC. Adverse reactions requiring
dosage reduction in >2% of patients who received INREBIC
included anemia (6%), diarrhea (3%), vomiting (3%), and
thrombocytopenia (2%).
DRUG INTERACTIONS:
Coadministration of INREBIC with a strong CYP3A4 inhibitor
increases fedratinib exposure. Increased exposure may increase the
risk of adverse reactions. Consider alternative therapies that do
not strongly inhibit CYP3A4 activity. Alternatively, reduce the
dose of INREBIC when administering with a strong CYP3A4 inhibitor.
Avoid INREBIC with strong and moderate CYP3A4 inducers. Avoid
INREBIC with dual CYP3A4 and CYP2C19 inhibitor. Coadministration of
INREBIC with drugs that are CYP3A4 substrates, CYP2C19 substrates,
or CYP2D6 substrates increases the concentrations of these drugs,
which may increase the risk of adverse reactions of these drugs.
Monitor for adverse reactions and adjust the dose of drugs that are
CYP3A4, CYP2C19, or CYP2D6 substrates as necessary when
coadministered with INREBIC.
PREGNANCY/LACTATION: Consider the benefits and risks of
INREBIC for the mother and possible risks to the fetus when
prescribing INREBIC to a pregnant woman. Due to the potential for
serious adverse reactions in a breastfed child, advise patients not
to breastfeed during treatment with INREBIC, and for at least 1
month after the last dose.
RENAL IMPAIRMENT: Reduce INREBIC dose when administered
to patients with severe renal impairment. No modification of the
starting dose is recommended for patients with mild to moderate
renal impairment. Due to potential increase of exposure, patients
with preexisting moderate renal impairment require more intensive
safety monitoring, and if necessary, dose modifications based on
adverse reactions.
HEPATIC IMPAIRMENT: Avoid use of INREBIC in patients with
severe hepatic impairment.
Please see full Prescribing Information, including Boxed
WARNING, and Summary of Product Characteristics for
INREBIC.
AUGTYRO
Augtyro (TPX-0005, BMS-986472) is a next-generation tyrosine
kinase inhibitor (TKI) targeting ROS1-positive or NTRK-positive
locally advanced or metastatic solid tumors, including non-small
cell lung cancer (NSCLC), where there remain significant unmet
medical needs for patients. Augtyro was designed to improve
durability of response and with favorable properties for human
brain penetration to enhance intracranial activity. It is being
studied in a registrational Phase 1/2 trial in adults (TRIDENT-1)
and a Phase 1/2 trial in pediatric patients (CARE).
Augtyro has demonstrated clinically meaningful results and was
granted three Breakthrough Therapy Designations (BTDs) by the FDA
for the treatment of patients with: ROS1-positive metastatic NSCLC
who have not been treated with a ROS1 TKI; ROS1-positive metastatic
NSCLC who have been previously treated with one ROS1 TKI and who
have not received prior platinum-based chemotherapy; and advanced
solid tumors that have an NTRK gene fusion who have progressed
following treatment with one or two prior tropomyosin receptor
kinase (TRK) TKIs (with or without prior chemotherapy) and have no
satisfactory alternative treatments.
Augtyro was also previously granted four fast-track designations
in patients with: ROS1-positive advanced NSCLC who have been
treated with disease progression following one prior line of
platinum-based chemotherapy and one prior line of a ROS1 TKI;
ROS1-positive advanced NSCLC who have not been treated with a ROS1
TKI; ROS1-positive advanced NSCLC who have been previously treated
with one ROS1 TKI and who have not received prior platinum-based
chemotherapy; and advanced solid tumors that have an NTRK gene
fusion who have progressed following treatment with at least one
prior line of chemotherapy and one or two prior TRK TKIs and have
no satisfactory alternative treatments. Augtyro was also granted an
Orphan Drug designation by the U.S. Food and Drug Administration
(FDA).
INDICATION
AUGTYROTM (repotrectinib) is indicated for the treatment of
adult patients with locally advanced or metastatic ROS1-positive
non-small cell lung cancer (NSCLC).
Warnings & Precautions
IMPORTANT SAFETY
INFORMATION
Central Nervous System Adverse Reactions
- Among the 351 patients who received AUGTYRO in the TRIDENT-1
study, a broad spectrum of central nervous system (CNS) adverse
reactions including dizziness, ataxia, and cognitive disorders
occurred in 75% with Grade 3 or 4 events occurring in 4%.
Dizziness, including vertigo, occurred in 64% and Grade 3 dizziness
occurred in 2.8% of patients. The median time to onset was 6 days
(1 day to 1.4 years). Dose interruption was required in 9% of
patients, and 12% required dose reduction of AUGTYRO due to
dizziness.
- Ataxia, including gait disturbance and balance disorder,
occurred in 29% of the 351 patients; Grade 3 ataxia occurred in
0.3%. The median time to onset was 15 days (1 day to 1.4 years).
Dose interruption was required in 6% of patients, 8% required dose
reduction and one patient (0.3%) permanently discontinued AUGTYRO
due to ataxia.
- Cognitive disorder, including memory impairment and disturbance
in attention, occurred in 23% of the 351 patients. Cognitive
disorders included memory impairment (13%), disturbance in
attention (11%), and confusional state (2%); Grade 3 cognitive
disorders occurred in 0.9% of patients. The median time to onset of
cognitive disorders was 37 days (1 day to 1.4 years). Dose
interruption was required in 2% of patients, 1.7% required dose
reduction and 0.6% permanently discontinued AUGTYRO due to
cognitive adverse reactions.
- Mood disorders occurred in 6% of the 351 patients. Mood
disorders occurring in >1% of patients included anxiety (2.8%),
irritability (1.1%), and depression (1.4%); Grade 4 mood disorders
(mania) occurred in 0.3% of patients. Dose interruption was
required in 0.3% of patients and 0.3% required a dose reduction due
to mood disorders.
- Sleep disorders including insomnia and hypersomnia occurred in
15% of the 351 patients. Sleep disorders observed in >1% of
patients were somnolence (8%), insomnia (6%) and hypersomnia
(1.1%). Dose interruption was required in 0.9% of patients, and
0.3% required a dose reduction due to sleep disorders.
- The incidences of CNS adverse reactions reported were similar
in patients with and without CNS metastases.
- Advise patients not to drive or use machines if they are
experiencing CNS adverse reactions. Withhold and then resume at
same or reduced dose upon improvement, or permanently discontinue
AUGTYRO based on severity.
Interstitial Lung Disease (ILD)/Pneumonitis
- Among the 351 patients treated with AUGTYRO, ILD/pneumonitis
(pneumonitis [2.6%] and interstitial lung disease [0.3%]) occurred
in 2.9%; Grade 3 ILD/pneumonitis occurred in 1.1%. The median time
to onset was 45 days (19 days to 0.9 years). Dose interruption was
required in 1.4% of patients, 0.6% required dose reduction, and
1.1% permanently discontinued AUGTYRO due to ILD/pneumonitis.
- Monitor patients for new or worsening pulmonary symptoms
indicative of ILD/pneumonitis. Immediately withhold AUGTYRO in
patients with suspected ILD/pneumonitis and permanently discontinue
AUGTYRO if ILD/pneumonitis is confirmed.
Hepatotoxicity
- Among the 351 patients treated with AUGTYRO, increased alanine
transaminase (ALT) occurred in 35%, increased aspartate
aminotransferase (AST) occurred in 40%, including Grade 3 or 4
increased ALT in 2% and increased AST in 2.6%. The median time to
onset of increased ALT or AST was 15 days (range: 1 day to 1.9
years). Increased ALT or AST leading to dose interruptions or
reductions occurred in 2.8% and 1.4% of patients, respectively.
Hyperbilirubinemia leading to dose interruptions occurred in
0.6%.
- Monitor liver function tests, including ALT, AST and bilirubin,
every 2 weeks during the first month of treatment, then monthly
thereafter and as clinically indicated. Withhold and then resume at
same or reduced dose upon improvement or permanently discontinue
AUGTYRO based on the severity.
Myalgia with Creatine Phosphokinase (CPK) Elevation
- Among the 351 patients treated with AUGTYRO, myalgia occurred
in 13% of patients, with Grade 3 in 0.6%. Median time to onset of
myalgia was 19 days (range: 1 day to 2 years). Concurrent increased
CPK within a 7-day window was observed in 3.7% of patients. AUGTYRO
was interrupted in one patient with myalgia and concurrent CPK
elevation.
- Advise patients to report any unexplained muscle pain,
tenderness, or weakness. Monitor serum CPK levels during AUGTYRO
treatment and monitor CPK levels every 2 weeks during the first
month of treatment and as needed in patients reporting unexplained
muscle pain, tenderness, or weakness. Initiate supportive care as
clinically indicated. Based on severity, withhold and then resume
AUGTYRO at same or reduced dose upon improvement.
Hyperuricemia
- Among the 351 patients treated with AUGTYRO, 18 patients (5%)
experienced hyperuricemia reported as an adverse reaction, 0.9%
experienced Grade 3 or 4 hyperuricemia. One patient without
pre-existing gout required urate-lowering medication.
- Monitor serum uric acid levels prior to initiating AUGTYRO and
periodically during treatment. Initiate treatment with
urate-lowering medications as clinically indicated. Withhold and
then resume at same or reduced dose upon improvement, or
permanently discontinue AUGTYRO based on severity.
Skeletal Fractures
- Among 351 adult patients who received AUGTYRO, fractures
occurred in 2.3%. Fractures involved the ribs (0.6%), feet (0.6%),
spine (0.3%), acetabulum (0.3%), sternum (0.3%), and ankles (0.3%).
Some fractures occurred at sites of disease and prior radiation
therapy. The median time to fracture was 71 days (range: 31 days to
1.4 years). AUGTYRO was interrupted in 0.3% of patients.
- Promptly evaluate patients with signs or symptoms (e.g., pain,
changes in mobility, deformity) of fractures. There are no data on
the effects of AUGTYRO on healing of known fractures and risk of
future fractures.
Embryo-Fetal Toxicity
- Based on literature reports in humans with congenital mutations
leading to changes in tropomyosin receptor tyrosine kinase (TRK)
signaling, findings from animal studies, and its mechanism of
action, AUGTYRO can cause fetal harm when administered to a
pregnant woman.
- Advise pregnant women of the potential risk to a fetus. Advise
females of reproductive potential to use effective non-hormonal
contraception during treatment with AUGTYRO and for 2 months
following the last dose, since AUGTYRO can render some hormonal
contraceptives ineffective.
- Advise male patients with female partners of reproductive
potential to use effective contraception during treatment with
AUGTYRO and for 4 months after the last dose.
Adverse Reactions
- Among 351 patients who received AUGTYRO for ROS1-positive NSCLC
and other solid tumors in the TRIDENT-1 trial, the most common
(>20%) adverse reactions were dizziness (64%), dysgeusia (50%),
peripheral neuropathy (47%), constipation (37%), dyspnea (30%),
ataxia (29%), fatigue (29%), cognitive disorders (23%), and nausea
(20%).
- In a subset of 264 patients who received AUGTYRO for
ROS1-positive NSCLC, the most common (≥20%) adverse reactions were
dizziness (63%), dysgeusia (48%), peripheral neuropathy (47%),
constipation (36%), dyspnea (30%), ataxia (28%), fatigue (24%),
cognitive disorders (23%), and muscular weakness (21%).
Drug Interactions
Effects of Other Drugs on AUGTYRO
Strong and Moderate CYP3A
Inhibitors
- Avoid concomitant use with strong or moderate CYP3A inhibitors.
Concomitant use of AUGTYRO with a strong or a moderate CYP3A
inhibitor may increase repotrectinib exposure, which may increase
the incidence and severity of adverse reactions of AUGTYRO.
Discontinue CYP3A inhibitors for 3 to 5 elimination half-lives of
the CYP3A inhibitor prior to initiating AUGTYRO.
P-gp Inhibitors
- Avoid concomitant use with P-gp inhibitors. Concomitant use of
AUGTYRO with a P-gp inhibitor may increase repotrectinib exposure,
which may increase the incidence and severity of adverse reactions
of AUGTYRO.
Strong and Moderate CYP3A
Inducers
- Avoid concomitant use with strong or moderate CYP3A inducers.
Concomitant use of AUGTYRO with a strong or moderate CYP3A inducer
may decrease repotrectinib plasma concentrations, which may
decrease efficacy of AUGTYRO.
Effects of AUGTYRO on other Drugs
Certain CYP3A4 Substrates
- Avoid concomitant use unless otherwise recommended in the
Prescribing Information for CYP3A substrates, where minimal
concentration changes can cause reduced efficacy. If concomitant
use is unavoidable, increase the CYP3A4 substrate dosage in
accordance with approved product labeling.
- Repotrectinib is a CYP3A4 inducer. Concomitant use of
repotrectinib decreases the concentration of CYP3A4 substrates,
which can reduce the efficacy of these substrates.
Contraceptives
- Repotrectinib is a CYP3A4 inducer, which can decrease progestin
or estrogen exposure to an extent that could reduce the
effectiveness of hormonal contraceptives.
- Avoid concomitant use of AUGTYRO with hormonal contraceptives.
Advise females to use an effective nonhormonal contraceptive.
Please see U.S. Full Prescribing Information for
AUGTYRO.
About the Bristol Myers Squibb and Ono
Pharmaceutical Collaboration
In 2011, through a collaboration agreement with Ono
Pharmaceutical Co., Bristol Myers Squibb expanded its territorial
rights to develop and commercialize Opdivo globally, except in
Japan, South Korea and Taiwan, where Ono had retained all rights to
the compound at the time. On July 23, 2014, Ono and Bristol Myers
Squibb further expanded the companies’ strategic collaboration
agreement to jointly develop and commercialize multiple
immunotherapies - as single agents and combination regimens - for
patients with cancer in Japan, South Korea and Taiwan.
About Bristol Myers Squibb and 2seventy
bio
Abecma is being jointly developed and commercialized in the U.S.
as part of a Co-Development, Co-Promotion, and Profit Share
Agreement between Bristol Myers Squibb and 2seventy bio. Bristol
Myers Squibb assumes sole responsibility for Abecma drug product
manufacturing and commercialization outside of the U.S. The
companies’ broad clinical development program for Abecma includes
ongoing and planned clinical studies (KarMMa-2, KarMMa-3, KarMMa-9)
for patients with multiple myeloma. For more information visit
clinicaltrials.gov.
About Bristol Myers
Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose
mission is to discover, develop and deliver innovative medicines
that help patients prevail over serious diseases. For more
information about Bristol Myers Squibb, visit us at BMS.com or
follow us on LinkedIn, Twitter, YouTube, Facebook and
Instagram.
Cautionary Statement Regarding
Forward-Looking Statements
This press release contains “forward-looking statements” within
the meaning of the Private Securities Litigation Reform Act of 1995
regarding, among other things, the research, development and
commercialization of pharmaceutical products. All statements that
are not statements of historical facts are, or may be deemed to be,
forward-looking statements. Such forward-looking statements are
based on current expectations and projections about our future
financial results, goals, plans and objectives and involve inherent
risks, assumptions and uncertainties, including internal or
external factors that could delay, divert or change any of them in
the next several years, that are difficult to predict, may be
beyond our control and could cause our future financial results,
goals, plans and objectives to differ materially from those
expressed in, or implied by, the statements. These risks,
assumptions, uncertainties and other factors include, among others,
that future study results may not be consistent with the results to
date, that the treatments and combination treatments may not
receive regulatory approval for the indications described in this
release will be commercially successful, and any marketing
approvals, if granted, may have significant limitations on their
use, and, if approved, whether the treatments and combination
treatments for such indications described in this release will be
commercially successful. No forward-looking statement can be
guaranteed. Forward-looking statements in this press release should
be evaluated together with the many risks and uncertainties that
affect Bristol Myers Squibb’s business and market, particularly
those identified in the cautionary statement and risk factors
discussion in Bristol Myers Squibb’s Annual Report on Form 10-K for
the year ended December 31, 2023, as updated by our subsequent
Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and
other filings with the Securities and Exchange Commission. The
forward-looking statements included in this document are made only
as of the date of this document and except as otherwise required by
applicable law, Bristol Myers Squibb undertakes no obligation to
publicly update or revise any forward-looking statement, whether as
a result of new information, future events, changed circumstances
or otherwise.
corporatefinancial-news
View source
version on businesswire.com: https://www.businesswire.com/news/home/20240522033055/en/
Bristol Myers Squibb
Media Inquiries: media@bms.com
Investors: investor.relations@bms.com
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
Von Dez 2024 bis Jan 2025
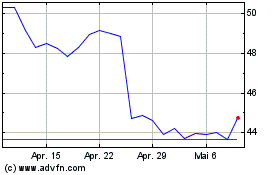
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
Von Jan 2024 bis Jan 2025