Bristol Myers Squibb (NYSE: BMY) today announced an update
following the initial analysis of results from the first of two
induction studies in the Phase 3 YELLOWSTONE clinical trial program
evaluating Zeposia (ozanimod) in adult patients with moderate to
severe active Crohn’s disease. The study did not meet its primary
endpoint of clinical remission at Week 12.
The safety profile of Zeposia in this study was consistent with
that observed in previously reported trials. The company will
complete a full evaluation of the YELLOWSTONE trial data and work
with investigators to share the results with the scientific
community in the future.
“To date, no S1P modulator has shown an effect in a Phase 3
trial in Crohn’s disease, where a high unmet medical need remains
for new therapies that offer more patients relief from symptoms and
the potential for remission,” said Roland Chen, MD, senior vice
president and head, Immunology, Cardiovascular and Neuroscience
development, Bristol Myers Squibb. “While we are disappointed that
the primary endpoint was not reached in this first induction trial,
we are committed to driving transformative science on behalf of
individuals with immune-mediated diseases and would like to thank
the investigators and patients who are participating in the
YELLOWSTONE clinical trial program.”
About the YELLOWSTONE Clinical Trial Program
YELLOWSTONE is a Phase 3, multicenter clinical trial program
consisting of two 12-week induction studies, a 52-week maintenance
study and a 264-week open-label extension study. YELLOWSTONE is
designed to evaluate the safety and efficacy of Zeposia (ozanimod)
administered orally to patients with Crohn’s disease versus
placebo. The induction studies include approximately 600 patients
each, with responders moving on to participate in the maintenance
study. Nonresponders, those with disease relapse during
maintenance, and completers of the maintenance study have the
option to enroll in the open-label extension trial. Patients in the
trial program are receiving Zeposia 0.92 mg (equivalent to 1
mg).
The primary endpoint of the induction studies is the proportion
of patients with a Crohn’s Disease Activity Index (CDAI) score of
less than 150. The co-primary endpoints of the maintenance study
are the proportion of patients with a CDAI score of less than 150
and the proportion of patients with a Simple Endoscopic Score for
Crohn’s disease (SES-CD) score decrease from baseline of at least
50%.
About Crohn’s disease
Crohn's disease is a chronic inflammatory bowel disease (IBD)
affecting the digestive tract. IBD results in the swelling or
inflammation of the intestines, which may result in permanent
damage and impact everyday life during disease flares. It is
estimated that approximately 12.6 million people worldwide have
IBD.
For many patients, Crohn’s disease occurs in the colon or the
third segment of the small intestine, the ileum, but may occur in
any part of the intestinal tract. Signs and symptoms of Crohn’s
disease can range from mild to severe. Most often, symptoms appear
gradually but can sometimes develop suddenly or without warning.
Patients with Crohn’s disease may experience ongoing disease
symptoms, or have episodes of symptom-free remission, which can be
followed by relapse or flares. Patients with Crohn's disease are
also at an increased risk of developing colorectal cancer. Living
with Crohn’s disease may severely affect quality of life both
physically and psychologically, particularly during disease flares
and relapses.
Bristol Myers Squibb: Pioneering Paths Forward in Immunology
to Transform Patients’ Lives
Bristol Myers Squibb is inspired by a single vision –
transforming patients’ lives through science. For people living
with immune-mediated diseases, the debilitating reality of enduring
chronic symptoms and disease progression can take a toll on their
physical, emotional and social well-being, making simple tasks and
daily life a challenge. Driven by our deep understanding of the
immune system that spans over 20 years of experience, and our
passion to help patients, the company continues to pursue
pathbreaking science with the goal of delivering meaningful
solutions that address unmet needs in rheumatology,
gastroenterology, dermatology and pulmonology. We follow the
science, aiming to tailor therapies to individual needs, improve
outcomes and expand treatment options by working to identify
mechanisms with the potential to achieve long-term remission – and
perhaps even cures – in the future. By building partnerships with
researchers, patients and caregivers to deliver innovative
treatments, Bristol Myers Squibb strives to elevate patient care to
new standards and deliver what matters most – the promise of living
a better life.
About Zeposia (ozanimod)
Zeposia (ozanimod) is an oral, sphingosine 1-phosphate (S1P)
receptor modulator that binds with high affinity to S1P receptors 1
and 5. Zeposia blocks the capacity of lymphocytes to egress from
lymph nodes, reducing the number of lymphocytes in peripheral
blood. The mechanism by which Zeposia exerts therapeutic effects in
Crohn’s disease is unknown but may involve the reduction of
lymphocyte migration into the gut.
Zeposia is approved in numerous countries around the world for
the treatment of adults with relapsing forms of MS and adults with
moderately to severely active ulcerative colitis.
U.S. FDA APPROVED INDICATIONS
ZEPOSIA® (ozanimod) is indicated for the treatment of:
- Relapsing forms of multiple sclerosis (MS), to include
clinically isolated syndrome, relapsing-remitting disease, and
active secondary progressive disease, in adults.
- Moderately to severely active ulcerative colitis (UC) in
adults.
IMPORTANT SAFETY INFORMATION
Contraindications:
- Patients who in the last 6 months, experienced myocardial
infarction, unstable angina, stroke, transient ischemic attack
(TIA), decompensated heart failure requiring hospitalization, or
Class III/IV heart failure or have a presence of Mobitz type II
second-degree or third-degree atrioventricular (AV) block, sick
sinus syndrome, or sino-atrial block, unless the patient has a
functioning pacemaker
- Patients with severe untreated sleep apnea
- Patients taking a monoamine oxidase (MAO) inhibitor
Infections: ZEPOSIA may increase the susceptibility to
infections. Life-threatening and rare fatal infections have
occurred in patients receiving ZEPOSIA. Obtain a recent (i.e.,
within 6 months or after discontinuation of prior MS or UC therapy)
complete blood count (CBC) including lymphocyte count before
initiation of ZEPOSIA. Delay initiation of ZEPOSIA in patients with
an active infection until the infection is resolved. Consider
interruption of treatment with ZEPOSIA if a patient develops a
serious infection. Continue monitoring for infections up to 3
months after discontinuing ZEPOSIA.
- Herpes zoster was reported as an adverse reaction in
ZEPOSIA-treated patients. Herpes simplex encephalitis and varicella
zoster meningitis have been reported with sphingosine 1-phosphate
(S1P) receptor modulators. Patients without a healthcare
professional-confirmed history of varicella (chickenpox), or
without documentation of a full course of vaccination against
varicella zoster virus (VZV), should be tested for antibodies to
VZV before initiating ZEPOSIA. A full course of vaccination for
antibody-negative patients with varicella vaccine is recommended
prior to commencing treatment with ZEPOSIA.
- Cases of fatal cryptococcal meningitis (CM) were reported in
patients treated with another S1P receptor modulator. If CM is
suspected, ZEPOSIA should be suspended until cryptococcal infection
has been excluded. If CM is diagnosed, appropriate treatment should
be initiated.
- In the MS and UC clinical studies, patients who received
ZEPOSIA were not to receive concomitant treatment with
antineoplastic, non-corticosteroid immunosuppressive, or
immune-modulating therapies used for treatment of MS and UC.
Concomitant use of ZEPOSIA with any of these therapies would be
expected to increase the risk of immunosuppression. When switching
to ZEPOSIA from immunosuppressive medications, consider the
duration of their effects and their mode of action to avoid
unintended additive immunosuppressive effects.
- Use of live attenuated vaccines should be avoided during and
for 3 months after treatment with ZEPOSIA. If live attenuated
vaccine immunizations are required, administer at least 1 month
prior to initiation of ZEPOSIA.
Progressive Multifocal Leukoencephalopathy (PML): PML is
an opportunistic viral infection of the brain that typically occurs
in patients who are immunocompromised, and that usually leads to
death or severe disability.
PML has been reported in patients treated with S1P receptor
modulators, including ZEPOSIA, and other MS and UC therapies and
has been associated with some risk factors. If PML is suspected,
withhold ZEPOSIA and perform an appropriate diagnostic
evaluation.
If confirmed, treatment with ZEPOSIA should be discontinued.
Immune reconstitution inflammatory syndrome (IRIS) has been
reported in MS patients treated with S1P receptor modulators who
developed PML and subsequently discontinued treatment. IRIS
presents as a clinical decline in the patient’s condition that may
be rapid, can lead to serious neurological complications or death,
and is often associated with characteristic changes on MRI. The
time to onset of IRIS in patients with PML was generally within a
few months after S1P receptor modulator discontinuation. Monitoring
for development of IRIS and appropriate treatment of the associated
inflammation should be undertaken.
Bradyarrhythmia and Atrioventricular Conduction Delays:
Since initiation of ZEPOSIA may result in a transient decrease in
heart rate and atrioventricular conduction delays, dose titration
is recommended to help reduce cardiac effects. Initiation of
ZEPOSIA without dose escalation may result in greater decreases in
heart rate. If treatment with ZEPOSIA is considered, advice from a
cardiologist should be sought for those individuals:
- with significant QT prolongation
- with arrhythmias requiring treatment with Class 1a or III
anti-arrhythmic drugs
- with ischemic heart disease, heart failure, history of cardiac
arrest or myocardial infarction, cerebrovascular disease, and
uncontrolled hypertension
- with a history of Mobitz type II second-degree or higher AV
block, sick sinus syndrome, or sino-atrial heart block
Liver Injury: Elevations of aminotransferases may occur
in patients receiving ZEPOSIA. Obtain liver function tests, if not
recently available (i.e., within 6 months), before initiation of
ZEPOSIA. Patients who develop symptoms suggestive of hepatic
dysfunction should have hepatic enzymes checked and ZEPOSIA should
be discontinued if significant liver injury is confirmed.
Fetal Risk: There are no adequate and well-controlled
studies in pregnant women. Based on animal studies, ZEPOSIA may
cause fetal harm. Women of childbearing potential should use
effective contraception to avoid pregnancy during treatment and for
3 months after stopping ZEPOSIA. Women who become pregnant while
taking ZEPOSIA for MS may enroll in the ZEPOSIA pregnancy registry
by calling 1-877-301-9314 or visiting
www.zeposiapregnancyregistry.com.
Increased Blood Pressure: Increase in systolic pressure
was observed after about 3 months of treatment and persisted
throughout treatment. Blood pressure should be monitored during
treatment and managed appropriately. Certain foods that may contain
very high amounts of tyramine could cause severe hypertension in
patients taking ZEPOSIA. Patients should be advised to avoid foods
containing a very large amount of tyramine while taking
ZEPOSIA.
Respiratory Effects: ZEPOSIA may cause a decline in
pulmonary function. Spirometric evaluation of respiratory function
should be performed during therapy, if clinically indicated.
Macular Edema: S1P modulators have been associated with
an increased risk of macular edema. Patients with a history of
uveitis or diabetes mellitus are at increased risk. Patients with a
history of these conditions should have an ophthalmic evaluation of
the fundus, including the macula, prior to treatment initiation and
regular follow-up examinations. An ophthalmic evaluation is
recommended in all patients at any time if there is a change in
vision. Continued use of ZEPOSIA in patients with macular edema has
not been evaluated; potential benefits and risks for the individual
patient should be considered if deciding whether ZEPOSIA should be
discontinued.
Posterior Reversible Encephalopathy Syndrome (PRES): Rare
cases of PRES have been reported in patients receiving a S1P
receptor modulator. If a ZEPOSIA-treated patient develops
unexpected neurological or psychiatric symptoms or any symptom/sign
suggestive of an increase in intracranial pressure, a complete
physical and neurological examination should be conducted. Symptoms
of PRES are usually reversible but may evolve into ischemic stroke
or cerebral hemorrhage. Delay in diagnosis and treatment may lead
to permanent neurological sequelae. If PRES is suspected, treatment
with ZEPOSIA should be discontinued.
Unintended Additive Immunosuppressive Effects From Prior
Immunosuppressive or Immune-Modulating Drugs: When switching
from drugs with prolonged immune effects, the half-life and mode of
action of these drugs must be considered to avoid unintended
additive immunosuppressive effects while at the same time
minimizing risk of disease reactivation. Initiating treatment with
ZEPOSIA after treatment with alemtuzumab is not recommended.
Severe Increase in Multiple Sclerosis (MS) Disability After
Stopping ZEPOSIA: In MS, severe exacerbation of disease,
including disease rebound, has been rarely reported after
discontinuation of a S1P receptor modulator. The possibility of
severe exacerbation of disease should be considered after stopping
ZEPOSIA treatment so patients should be monitored upon
discontinuation. After stopping ZEPOSIA in the setting of PML,
monitor for development of immune reconstitution inflammatory
syndrome (PML-IRIS).
Immune System Effects After Stopping ZEPOSIA: After
discontinuing ZEPOSIA, the median time for lymphocyte counts to
return to the normal range was 30 days with approximately 90% of
patients in the normal range within 3 months. Use of
immunosuppressants within this period may lead to an additive
effect on the immune system, therefore caution should be applied
when initiating other drugs 4 weeks after the last dose of
ZEPOSIA.
Most Common Adverse Reactions that occurred in the MS
clinical trials of ZEPOSIA-treated patients (≥4%): upper
respiratory infection, hepatic transaminase elevation, orthostatic
hypotension, urinary tract infection, back pain, and
hypertension.
In the UC clinical trials, the most common adverse reactions
that occurred in ≥4% of ZEPOSIA-treated patients and greater than
in patients who received placebo were upper respiratory infection,
liver test increased, and headache.
Use in Specific Populations: Hepatic Impairment: Dosage
adjustment in patients with mild or moderate hepatic impairment
(Child-Pugh class A or B) is required, and use of ZEPOSIA in
patients with severe hepatic impairment (Child-Pugh class C) is not
recommended.
For additional safety information, please see the full
Prescribing Information and Medication
Guide.
About Bristol Myers Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose
mission is to discover, develop and deliver innovative medicines
that help patients prevail over serious diseases. For more
information about Bristol Myers Squibb, visit us at BMS.com or
follow us on LinkedIn, Twitter, YouTube, Facebook and
Instagram.
Cautionary Statement Regarding Forward-Looking
Statements
This press release contains “forward-looking statements” within
the meaning of the Private Securities Litigation Reform Act of 1995
regarding, among other things, the research, development and
commercialization of pharmaceutical products. All statements that
are not statements of historical facts are, or may be deemed to be,
forward-looking statements. Such forward-looking statements are
based on historical performance and current expectations and
projections about our future financial results, goals, plans and
objectives and involve inherent risks, assumptions and
uncertainties, including internal or external factors that could
delay, divert or change any of them in the next several years, that
are difficult to predict, may be beyond our control and could cause
our future financial results, goals, plans and objectives to differ
materially from those expressed in, or implied by, the statements.
These risks, assumptions, uncertainties and other factors include,
among others, the possibility of unfavorable results from further
clinical trials involving Zeposia (ozanimod) and whether Zeposia
for the additional indication described in this release will be
successfully developed and commercialized. No forward-looking
statement can be guaranteed. Forward-looking statements in this
press release should be evaluated together with the many risks and
uncertainties that affect Bristol Myers Squibb’s business and
market, particularly those identified in the cautionary statement
and risk factors discussion in Bristol Myers Squibb’s Annual Report
on Form 10-K for the year ended December 31, 2023, as updated by
our subsequent Quarterly Reports on Form 10-Q, Current Reports on
Form 8-K and other filings with the Securities and Exchange
Commission. The forward-looking statements included in this
document are made only as of the date of this document and except
as otherwise required by applicable law, Bristol Myers Squibb
undertakes no obligation to publicly update or revise any
forward-looking statement, whether as a result of new information,
future events, changed circumstances or otherwise.
corporatefinancial-news
View source
version on businesswire.com: https://www.businesswire.com/news/home/20240327817166/en/
Bristol Myers Squibb Media Inquiries:
media@bms.com Investors: investor.relations@bms.com
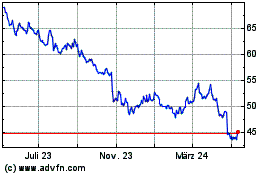
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
Von Jan 2025 bis Feb 2025
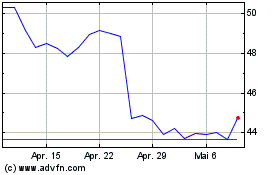
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
Von Feb 2024 bis Feb 2025