Abecma demonstrated superiority over
standard regimens in the Phase 3 KarMMa-3 trial, with a 51%
reduction in risk of disease progression or death and a
well-established safety profile with mostly low-grade and transient
occurrences of cytokine release syndrome and neurotoxicity
Approval reinforces Bristol Myers Squibb’s
commitment to bring the transformative potential of cell therapy
into earlier lines of treatment
Bristol Myers Squibb (NYSE: BMY) today announced that the
European Commission (EC) has granted approval to Abecma®
(idecabtagene vicleucel; ide-cel) for the treatment of adult
patients with relapsed and refractory multiple myeloma who have
received at least two prior therapies, including an
immunomodulatory agent (IMiD), a proteasome inhibitor (PI), and an
anti-CD38 antibody and have demonstrated disease progression on the
last therapy. Abecma is the first chimeric antigen receptor (CAR) T
cell immunotherapy approved in the European Union (EU) for use in
earlier lines of therapy for relapsed and refractory multiple
myeloma. This expanded approval of Abecma covers all EU member
states.* In the EU, Abecma has maintained its Orphan Designation
for the treatment of multiple myeloma.
“Today’s approval in the European Union marks an exciting
milestone in our efforts to bring the transformative potential of
cell therapies into earlier lines of treatment,” said Monica Shaw,
M.D., senior vice president and head of European Markets, Bristol
Myers Squibb. “Abecma is an important treatment option for patients
with triple-class exposed relapsed and refractory multiple myeloma
who have received at least two prior therapies and is leading the
way toward a promising shift in the treatment paradigm.”
The current treatment paradigm for multiple myeloma includes
IMiDs, PIs, and anti-CD38 monoclonal antibodies; however, many
patients go on to relapse and/or become refractory to these classes
of therapy. With increased use of the three main classes of therapy
as combination regimens, more patients are becoming triple-class
exposed earlier in their treatment journey. There have historically
been limited options for patients with triple-class exposed
relapsed and/or refractory multiple myeloma, and patients tend to
have poor outcomes with a median progression-free survival of three
to five months.
“As patients with multiple myeloma become exposed to the three
main classes of therapy earlier in treatment and still experience
relapsed and/or refractory disease, it is critical that we continue
to add innovative treatment options to our arsenal that can
potentially provide long-term disease control,” said Paula
Rodriguez-Otero, M.D., Ph.D., Department of Hematology, Clinica
Universidad de Navarra, Pamplona, Spain. “This expanded approval of
ide-cel represents key progress in bringing a personalized therapy
that delivers significantly improved, durable outcomes to patients
with triple-class exposed relapsed and refractory multiple myeloma
after two prior therapies.”
With a significant increase in manufacturing capacity and over
90% manufacturing success rate globally, Bristol Myers Squibb is
prepared to meet increased demand for Abecma. The company is
focused on making Abecma available in the EU for this indication,
including completion of reimbursement procedures.
Based on the KarMMa-3 study, Abecma is also the first cell
therapy approved in Switzerland for the treatment of adult patients
with relapsed and refractory multiple myeloma who have received at
least two prior lines of therapies and the first cell therapy
approved in Japan for adult patients with triple-class exposed
relapsed or refractory multiple myeloma after two prior lines of
therapy.
Abecma is also approved in the U.S. for adult patients with
triple-class exposed relapsed or refractory multiple myeloma after
four or more prior lines of therapy and approved in Great Britain
and Israel for adult patients with triple-class exposed relapsed
and refractory multiple myeloma after three or more prior lines of
therapy. A supplemental Biologics License Application for Abecma
for triple-class exposed relapsed and refractory multiple myeloma
is currently under review with the U.S. Food and Drug
Administration (FDA). The FDA’s Oncologic Drugs Advisory Committee
(ODAC) recently voted positively that Abecma demonstrated a
favorable benefit/risk profile for patients with triple-class
exposed relapsed or refractory multiple myeloma based on results
from the pivotal Phase 3 KarMMa-3 study.
*Centralized Marketing Authorization does not include approval
in Great Britain (England, Scotland and Wales).
Abecma KarMMa-3 Clinical Trial Results
The EC approval of Abecma is based on results from KarMMa-3, a
pivotal Phase 3, open-label, global, randomized controlled study
evaluating Abecma compared to standard combination regimens in
patients with relapsed and refractory multiple myeloma who received
two to four prior lines of treatment, including an IMiD, a PI, and
an anti-CD38 monoclonal antibody (triple-class exposed), and who
were refractory to the last treatment regimen.
At a pre-specified interim analysis with a median follow-up of
18.6 months, treatment with Abecma (n=254) significantly improved
progression-free survival (PFS), the study’s primary endpoint,
compared to standard regimens (n=132), with a median PFS of 13.8
months (95% CI: 11.8-16.1) versus 4.4 months (95% CI: 3.4-5.8) (HR:
0.49 [95% CI: 0.38-0.63]; p<0.0001), representing a 51%
reduction in the risk of disease progression or death. Results from
the primary analysis, with a median follow-up of 30.9 months, were
consistent with the interim analysis and represent the longest
follow-up for a randomized Phase 3 CAR T cell therapy in this
patient population. Treatment with Abecma also showed a significant
improvement in overall response rate (ORR) with the majority (71.3%
[95% CI: 65.7-76.8]) of patients treated with Abecma achieving a
response, and 43.7% achieving a complete or stringent complete
response. In comparison, less than half of patients (42.4% [95% CI:
34-50.9]) who received standard regimens achieved a response, with
5.3% experiencing a complete response or stringent complete
response.
The KarMMa-3 trial had a patient-centric design that allowed for
crossover from standard regimens to Abecma upon confirmed disease
progression, with more than half (56%) of patients in the standard
regimens arm crossing over to receive Abecma as a subsequent
therapy, due to disease progression while receiving standard
regimens. Median overall survival (OS), a secondary endpoint of the
study, was 41.4 months with Abecma (95% CI: 30.9-NR) and 37.9
months with standard regimens (95% CI: 23.4-NR) (95% CI: 0.73-1.40;
HR: 1.01). Based on real-world evidence, median OS for patients
with triple-class exposed relapsed and refractory multiple myeloma
is approximately 13 months, underscoring the confounding impact
that crossover had on the median OS observed with standard regimens
in the KarMMa-3 trial.
Based on a pooled analysis of the KarMMa, CRB-401 and KarMMa-3
studies (n=409), Abecma has exhibited a well-established and
consistent safety profile with mostly low-grade and transient
occurrences of cytokine release syndrome (CRS) and neurotoxicity.
In patients treated with Abecma, any grade CRS has occurred in
84.6% of patients, with Grade ≥3 CRS occurring in 5.1% of patients
and fatal (Grade 5) CRS reported in 0.7% of patients. The median
time to onset of CRS was one day (range: 1 to 17) and the median
duration of CRS was four days (range: 1 to 63). In the KarMMa and
KarMMa-3 studies (n=353), any-grade neurotoxicity occurred in 16.1%
of patients, with Grade 3/4 neurotoxicity occurring in 3.1% of
patients, and no Grade 5 events reported. Median time to onset of
neurotoxicity was three days (range: 1-317 days) and median
duration of neurotoxicity was three days (range: 1-252 days). No
cases of Parkinsonism were reported.
About Abecma
Abecma is a CAR T cell therapy that recognizes and binds to the
B-cell maturation antigen (BCMA) on the surface of multiple myeloma
cells leading to CAR T cell proliferation, cytokine secretion, and
subsequent cytolytic killing of BCMA-expressing cells. Abecma is
the first-in-class BCMA-directed CAR T cell immunotherapy approved
by the U.S. FDA for the treatment of adult patients with relapsed
or refractory multiple myeloma after four or more prior lines of
therapy, including an immunomodulatory agent, a proteasome
inhibitor, and an anti-CD38 monoclonal antibody. Please see the
Important Safety Information section below, including Boxed
WARNINGS for Abecma regarding CRS, neurologic toxicities,
Hemophagocytic Lymphohistiocytosis/Macrophage Activation Syndrome
and Prolonged Cytopenia.
Abecma is being jointly developed and commercialized in the U.S.
as part of a Co-Development, Co-Promotion, and Profit Share
Agreement between Bristol Myers Squibb and 2seventy bio. Bristol
Myers Squibb assumes sole responsibility for Abecma drug product
manufacturing and commercialization outside of the U.S. The
companies’ broad clinical development program for Abecma includes
ongoing and planned clinical studies (KarMMa-2, KarMMa-9) for
patients with multiple myeloma. For more information visit
clinicaltrials.gov.
Full European Summary of Product Characteristics for Abecma is
available from the EMA website at www.ema.europa.eu.
Abecma U.S. FDA-Approved Indication
ABECMA® (idecabtagene vicleucel) is a B-cell maturation antigen
(BCMA)-directed genetically modified autologous T cell
immunotherapy indicated for the treatment of adult patients with
relapsed or refractory multiple myeloma after four or more prior
lines of therapy, including an immunomodulatory agent, a proteasome
inhibitor, and an anti-CD38 monoclonal antibody.
U.S. Important Safety
Information
BOXED WARNING: CYTOKINE RELEASE SYNDROME, NEUROLOGIC
TOXICITIES, HLH/MAS, AND PROLONGED CYTOPENIA
- Cytokine Release Syndrome (CRS), including fatal or
life-threatening reactions, occurred in patients following
treatment with ABECMA. Do not administer ABECMA to patients with
active infection or inflammatory disorders. Treat severe or
life-threatening CRS with tocilizumab or tocilizumab and
corticosteroids.
- Neurologic Toxicities, which may be severe or life-threatening,
occurred following treatment with ABECMA, including concurrently
with CRS, after CRS resolution, or in the absence of CRS. Monitor
for neurologic events after treatment with ABECMA. Provide
supportive care and/or corticosteroids as needed.
- Hemophagocytic Lymphohistiocytosis/Macrophage Activation
Syndrome (HLH/MAS) including fatal and life-threatening reactions,
occurred in patients following treatment with ABECMA. HLH/MAS can
occur with CRS or neurologic toxicities.
- Prolonged Cytopenia with bleeding and infection, including
fatal outcomes following stem cell transplantation for
hematopoietic recovery, occurred following treatment with
ABECMA.
- ABECMA is available only through a restricted program under a
Risk Evaluation and Mitigation Strategy (REMS) called the ABECMA
REMS.
WARNINGS AND PRECAUTIONS:
Cytokine Release Syndrome (CRS): CRS, including fatal or
life-threatening reactions, occurred following treatment with
ABECMA in 85% (108/127) of patients. Grade 3 or higher CRS occurred
in 9% (12/127) of patients, with Grade 5 CRS reported in one (0.8%)
patient. The median time to onset of CRS, any grade, was 1 day
(range: 1 - 23 days) and the median duration of CRS was 7 days
(range: 1 - 63 days). The most common manifestations included
pyrexia, hypotension, tachycardia, chills, hypoxia, fatigue, and
headache. Grade 3 or higher events that may be associated with CRS
include hypotension, hypoxia, hyperbilirubinemia,
hypofibrinogenemia, acute respiratory distress syndrome (ARDS),
atrial fibrillation, hepatocellular injury, metabolic acidosis,
pulmonary edema, multiple organ dysfunction syndrome, and
HLH/MAS.
Identify CRS based on clinical presentation. Evaluate for and
treat other causes of fever, hypoxia, and hypotension. CRS has been
reported to be associated with findings of HLH/MAS, and the
physiology of the syndromes may overlap. In patients with
progressive symptoms of CRS or refractory CRS despite treatment,
evaluate for evidence of HLH/MAS.
Fifty four percent (68/127) of patients received tocilizumab
(single dose: 35%; more than 1 dose: 18%). Overall, 15% (19/127) of
patients received at least 1 dose of corticosteroids for treatment
of CRS. All patients that received corticosteroids for CRS received
tocilizumab. Ensure that a minimum of 2 doses of tocilizumab are
available prior to infusion of ABECMA.
Monitor patients at least daily for 7 days following ABECMA
infusion at the REMS-certified healthcare facility for signs or
symptoms of CRS and monitor patients for signs or symptoms of CRS
for at least 4 weeks after ABECMA infusion. At the first sign of
CRS, institute treatment with supportive care, tocilizumab and/or
corticosteroids as indicated.
Counsel patients to seek immediate medical attention should
signs or symptoms of CRS occur at any time.
Neurologic Toxicities: Neurologic toxicities, including
immune effector cell-associated neurotoxicity syndrome (ICANS),
which may be severe or life- threatening, occurred concurrently
with CRS, after CRS resolution, or in the absence of CRS following
treatment with ABECMA. Neurologic toxicities occurred in 28%
(36/127) of patients receiving ABECMA, including Grade 3 in 4%
(5/127) of patients. One patient had ongoing Grade 2 neurotoxicity
at the time of death. Two patients had ongoing Grade 1 tremor at
the time of data cutoff. The median time to onset of neurotoxicity
was 2 days (range: 1 - 42 days). CAR T cell-associated
neurotoxicity resolved in 92% (33/36) of patients with a median
time to resolution of 5 days (range: 1 - 61 days). The median
duration of neurotoxicity was 6 days (range: 1 - 578) in all
patients including 3 patients with ongoing neurotoxicity.
Thirty-four patients with neurotoxicity had CRS with onset in 3
patients before, 29 patients during, and 2 patients after CRS. The
most frequently reported manifestations of CAR T cell-associated
neurotoxicity include encephalopathy, tremor, aphasia, and
delirium. Grade 4 neurotoxicity and cerebral edema in 1 patient,
Grade 3 myelitis, and Grade 3 parkinsonism have been reported with
ABECMA in another study in multiple myeloma.
Monitor patients at least daily for 7 days following ABECMA
infusion at the REMS-certified healthcare facility for signs or
symptoms of neurologic toxicities and monitor patients for signs or
symptoms of neurologic toxicities for at least 4 weeks after ABECMA
infusion and treat promptly. Rule out other causes of neurologic
symptoms. Neurologic toxicity should be managed with supportive
care and/or corticosteroids as needed.
Counsel patients to seek immediate medical attention should
signs or symptoms occur at any time.
Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage
Activation Syndrome (MAS): HLH/MAS occurred in 4% (5/127) of
patients receiving ABECMA. One patient developed fatal multi-organ
HLH/MAS with CRS and another patient developed fatal
bronchopulmonary aspergillosis with contributory HLH/MAS. Three
cases of Grade 2 HLH/MAS resolved. All events of HLH/MAS had onset
within 10 days of receiving ABECMA with a median onset of 7 days
(range: 4 - 9 days) and occurred in the setting of ongoing or
worsening CRS. Two patients with HLH/MAS had overlapping
neurotoxicity. The manifestations of HLH/MAS include hypotension,
hypoxia, multiple organ dysfunction, renal dysfunction, and
cytopenia. HLH/MAS is a potentially life-threatening condition with
a high mortality rate if not recognized early and treated.
Treatment of HLH/MAS should be administered per institutional
guidelines.
ABECMA REMS: Due to the risk of CRS and neurologic
toxicities, ABECMA is available only through a restricted program
under a Risk Evaluation and Mitigation Strategy (REMS) called the
ABECMA REMS. Further information is available at www.AbecmaREMS.com
or 1-888-423-5436.
Hypersensitivity Reactions: Allergic reactions may occur
with the infusion of ABECMA. Serious hypersensitivity reactions,
including anaphylaxis, may be due to dimethyl sulfoxide (DMSO) in
ABECMA.
Infections: ABECMA should not be administered to patients
with active infections or inflammatory disorders. Severe,
life-threatening, or fatal infections occurred in patients after
ABECMA infusion. Infections (all grades) occurred in 70% of
patients. Grade 3 or 4 infections occurred in 23% of patients.
Overall, 4 patients had Grade 5 infections (3%); 2 patients (1.6%)
had Grade 5 events of pneumonia, 1 patient (0.8%) had Grade 5
bronchopulmonary aspergillosis, and 1 patient (0.8%) had
cytomegalovirus (CMV) pneumonia associated with Pneumocystis
jirovecii. Monitor patients for signs and symptoms of infection
before and after ABECMA infusion and treat appropriately.
Administer prophylactic, pre-emptive, and/or therapeutic
antimicrobials according to standard institutional guidelines.
Febrile neutropenia was observed in 16% (20/127) of patients
after ABECMA infusion and may be concurrent with CRS. In the event
of febrile neutropenia, evaluate for infection and manage with
broad-spectrum antibiotics, fluids, and other supportive care.
Viral Reactivation: CMV infection resulting in pneumonia and
death has occurred following ABECMA administration. Monitor and
treat for CMV reactivation in accordance with clinical guidelines.
Hepatitis B virus (HBV) reactivation, in some cases resulting in
fulminant hepatitis, hepatic failure, and death, can occur in
patients treated with drugs directed against plasma cells. Perform
screening for CMV, HBV, hepatitis C virus (HCV), and human
immunodeficiency virus (HIV) in accordance with clinical guidelines
before collection of cells for manufacturing.
Prolonged Cytopenias: In the clinical study, 41% of
patients (52/127) experienced prolonged Grade 3 or 4 neutropenia
and 49% (62/127) experienced prolonged Grade 3 or 4
thrombocytopenia that had not resolved by Month 1 following ABECMA
infusion. In 83% (43/52) of patients who recovered from Grade 3 or
4 neutropenia after Month 1, the median time to recovery from
ABECMA infusion was 1.9 months. In 65% (40/62) of patients who
recovered from Grade 3 or 4 thrombocytopenia, the median time to
recovery was 2.1 months.
Three patients underwent stem cell therapy for hematopoietic
reconstitution due to prolonged cytopenia. Two of the three
patients died from complications of prolonged cytopenia. Monitor
blood counts prior to and after ABECMA infusion. Manage cytopenia
with myeloid growth factor and blood product transfusion
support.
Hypogammaglobulinemia: Hypogammaglobulinemia was reported
as an adverse event in 21% (27/127) of patients; laboratory IgG
levels fell below 500 mg/dl after infusion in 25% (32/127) of
patients treated with ABECMA.
Monitor immunoglobulin levels after treatment with ABECMA and
administer IVIG for IgG <400 mg/dl. Manage appropriately per
local institutional guidelines, including infection precautions and
antibiotic or antiviral prophylaxis.
The safety of immunization with live viral vaccines during or
after ABECMA treatment has not been studied. Vaccination with live
virus vaccines is not recommended for at least 6 weeks prior to the
start of lymphodepleting chemotherapy, during ABECMA treatment, and
until immune recovery following treatment with ABECMA.
Secondary Malignancies: Patients treated with ABECMA may
develop secondary malignancies. Monitor life-long for secondary
malignancies. If a secondary malignancy occurs, contact
Bristol-Myers Squibb at 1-888-805-4555 to obtain instructions on
patient samples to collect for testing of secondary malignancy of T
cell origin.
Effects on Ability to Drive and Operate Machinery: Due to
the potential for neurologic events, patients receiving ABECMA are
at risk for altered or decreased consciousness or coordination in
the 8 weeks following ABECMA infusion. Advise patients to refrain
from driving and engaging in hazardous occupations or activities,
such as operating heavy or potentially dangerous machinery, during
this initial period.
Adverse Reactions: The most common nonlaboratory adverse
reactions include CRS, infections – pathogen unspecified, fatigue,
musculoskeletal pain, hypogammaglobulinemia, diarrhea, upper
respiratory tract infection, nausea, viral infections,
encephalopathy, edema, pyrexia, cough, headache, and decreased
appetite.
Please see full Prescribing Information, including Boxed
WARNINGS and Medication Guide.
Bristol Myers Squibb: Creating a Better
Future for People with Cancer
Bristol Myers Squibb is inspired by a single vision —
transforming patients’ lives through science. The goal of the
company’s cancer research is to deliver medicines that offer each
patient a better, healthier life and to make cure a possibility.
Building on a legacy across a broad range of cancers that have
changed survival expectations for many, Bristol Myers Squibb
researchers are exploring new frontiers in personalized medicine
and, through innovative digital platforms, are turning data into
insights that sharpen their focus. Deep understanding of causal
human biology, cutting-edge capabilities and differentiated
research platforms uniquely position the company to approach cancer
from every angle.
Cancer can have a relentless grasp on many parts of a patient’s
life, and Bristol Myers Squibb is committed to taking actions to
address all aspects of care, from diagnosis to survivorship. As a
leader in cancer care, Bristol Myers Squibb is working to empower
all people with cancer to have a better future.
About Bristol Myers
Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose
mission is to discover, develop and deliver innovative medicines
that help patients prevail over serious diseases. For more
information about Bristol Myers Squibb, visit us at BMS.com or
follow us on LinkedIn, Twitter, YouTube, Facebook and
Instagram.
Forward-Looking Statement of Bristol
Myers Squibb
This press release contains “forward-looking statements” within
the meaning of the Private Securities Litigation Reform Act of 1995
regarding, among other things, the research, development and
commercialization of pharmaceutical products. All statements that
are not statements of historical facts are, or may be deemed to be,
forward-looking statements. Such forward-looking statements are
based on current expectations and projections about our future
financial results, goals, plans and objectives and involve inherent
risks, assumptions and uncertainties, including internal or
external factors that could delay, divert or change any of them in
the next several years, that are difficult to predict, may be
beyond our control and could cause our future financial results,
goals, plans and objectives to differ materially from those
expressed in, or implied by, the statements. These risks,
assumptions, uncertainties and other factors include, among others,
that the outcome of pricing and reimbursement negotiations in
individual countries in Europe may delay or limit the commercial
potential of Abecma® (idecabtagene vicleucel) for the additional
indication described in this release, any marketing approvals, if
granted, may have significant limitations on their use, and that
continued approval of Abecma for such additional indication
described in this release may be contingent upon verification and
description of clinical benefit in confirmatory trials, and whether
Abecma for such additional indication described in this release
will be commercially successful. No forward-looking statement can
be guaranteed. Forward-looking statements in this press release
should be evaluated together with the many risks and uncertainties
that affect Bristol Myers Squibb’s business and market,
particularly those identified in the cautionary statement and risk
factors discussion in Bristol Myers Squibb’s Annual Report on Form
10-K for the year ended December 31, 2023, as updated by our
subsequent Quarterly Reports on Form 10-Q, Current Reports on Form
8-K and other filings with the Securities and Exchange Commission.
The forward-looking statements included in this document are made
only as of the date of this document and except as otherwise
required by applicable law, Bristol Myers Squibb undertakes no
obligation to publicly update or revise any forward-looking
statement, whether as a result of new information, future events,
changed circumstances or otherwise.
corporatefinancial-news
View source
version on businesswire.com: https://www.businesswire.com/news/home/20240320035615/en/
Bristol Myers Squibb Media Inquiries:
media@bms.com Investors: investor.relations@bms.com
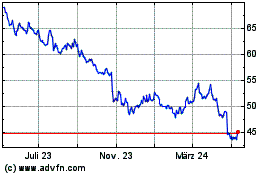
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
Von Jan 2025 bis Feb 2025
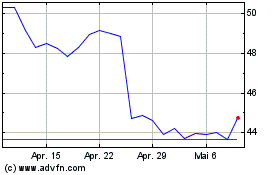
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
Von Feb 2024 bis Feb 2025