By Anna Wilde Mathews and Sarah Nassauer
This article is being republished as part of our daily
reproduction of WSJ.com articles that also appeared in the U.S.
print edition of The Wall Street Journal (January 16, 2019).
CVS Health Corp. is battling Walmart Inc. over the cost of
filling prescriptions, a clash that could result in a split between
the retail behemoth and the health-care giant.
Walmart is expected to leave CVS Caremark pharmacy networks over
the dispute, a split that could occur as soon as early February,
though CVS said it has asked for an extension through April 30. The
two sides could also still end up hammering out a deal, despite the
current public hostilities.
Different versions of how the dispute played out quickly
emerged.
CVS Caremark, the pharmacy-benefits unit of CVS Health, said
Monday that Walmart is seeking an increase in what the retailer
gets paid for prescriptions, which would "ultimately result in
higher costs for our clients and consumers." CVS Caremark, which is
separate from CVS's retail drugstores, reimburses pharmacies when
shoppers with CVS Caremark prescription coverage buy medicine.
But a person familiar with Walmart's position said Walmart
didn't ask CVS to increase the amount it pays the retailer when
shoppers fill a prescription. Walmart asked CVS to maintain rates
at current levels, said this person. In response, a CVS spokesman
pointed to the company's earlier statement.
Negotiations over rates reached a boiling point last week when
Walmart sent a contract termination letter to CVS, according to
people familiar with the situation. Walmart continued to negotiate
with CVS as recently as last Friday, said one of these people.
Walmart aims to continue discussions with CVS Caremark and is
"trying to find a solution that benefits all parties," said a
spokeswoman for the retailer. "We are committed to providing value
to our customers across our business, including our pharmacy, but
we don't want to give that value to the middleman.... Walmart is
standing up to CVS's behaviors that are putting pressure on
pharmacies and disrupting patient care."
The Walmart spokeswoman said problems can come up when a PBM has
strong power to influence where people can get their prescriptions
filled.
CVS said in its statement that it remains "open to continuing
timely good faith negotiations with Walmart in the hopes of
reaching an agreement to provide quality pharmacy care at a
reasonable cost."
If the two giants part ways, it will affect people whose
employers have CVS Caremark-administered drug benefits, as well as
Medicaid enrollees with CVS drug coverage. Their plans wouldn't pay
for prescriptions filled at Walmart. Walmart is one of the
country's largest retail pharmacy players, offering pharmacies in
nearly all of its approximately 4,600 U.S. stores.
CVS said it retains a large network of more than 63,000
pharmacies without Walmart, and less than 5% of its members
enrolled in affected plans use only Walmart for prescriptions.
But the impact could be heavier for the employees of clients in
rural areas and the South, where Walmart is a particularly
important presence, said Nadina Rosier, who is head of the pharmacy
practice at advisory firm Willis Towers Watson. "It truly depends
on your vantage point," she said. "If you're a member who works for
an employer where Walmart is the dominant player, you're going to
feel the pain."
The public spat shows how tensions are rising between
pharmacies, pharmacy-benefit managers and insurers amid steep
pressure from consumers, employers and politicians to stem rising
drug costs. Pharmacy-benefit managers, as well as drug
manufacturers, have come under scrutiny amid complaints about
opaque pricing practices, and PBMs are under pressure to wring out
more cost.
A similar high-profile battle between a pharmacy-benefit manager
and a pharmacy company played out in 2012, when millions of Express
Scripts Holding Co. customers had to switch prescriptions to
different pharmacies because Walgreen Co. dropped out of the PBM's
network. The clash was resolved after seven months.
Now, the issues are complicated by mergers that are creating new
competitive fault lines in the industry. CVS recently completed its
nearly $70 billion acquisition of health insurer Aetna, creating an
industry giant that combines a retail pharmacy, pharmacy-benefit
management and Aetna's insurance businesses. Insurer Cigna Corp.
also recently closed its $54 billion acquisition of Express
Scripts.
CVS is also closely aligned with Walmart competitor Target
Corp., buying up the pharmacies inside Target stores in 2015.
Walmart has considered diving deeper into the health-care space.
Last spring, Walmart held preliminary talks with health insurer
Humana Inc., The Wall Street Journal has reported, but those talks
have cooled.
CVS Caremark said the dispute with Walmart doesn't affect the
pharmacy networks in its Medicare plans, and the split also doesn't
involve Sam's Club stores, Walmart's chain of warehouse stores. The
issue won't materially impact CVS's financial results, it said.
Write to Anna Wilde Mathews at anna.mathews@wsj.com and Sarah
Nassauer at sarah.nassauer@wsj.com
(END) Dow Jones Newswires
January 16, 2019 02:47 ET (07:47 GMT)
Copyright (c) 2019 Dow Jones & Company, Inc.
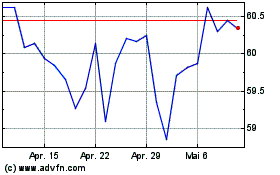
Walmart (NYSE:WMT)
Historical Stock Chart
Von Mär 2024 bis Apr 2024
Walmart (NYSE:WMT)
Historical Stock Chart
Von Apr 2023 bis Apr 2024
