Teva Pharmaceuticals, a U.S. affiliate of Teva Pharmaceutical
Industries Ltd. (NYSE and TASE: TEVA), and NATCO Pharma Limited
(NSE: NATCOPHARM; BSE: 524816), announced today the launch of
additional strengths for the generic version of Revlimid®1
(lenalidomide capsules), in 2.5 mg, and 20 mg strengths, in the
United States.
The companies have launched four other strengths of the product
in March 2022 in the US market. With today’s launch the companies
made available all the strengths of lenalidomide in the US
market.
Teva’s lenalidomide capsules are a prescription medicine used in
adults for the treatment of (i) multiple myeloma in combination
with the medicine dexamethasone, (ii) certain myelodysplastic
syndromes, and (iii) mantle cell lymphoma following specific prior
treatment. Please see the below “What are lenalidomide capsules?”
section for more information.
“The launch of additional strengths for the generic version of
Revlimid® in the U.S. enhances access to an important treatment
option for patients, and further demonstrates Teva’s commitment to
making generic drugs available to the patients who need them,” said
Christine Baeder, SVP, Chief Operating Officer, US Generics and
Biosimilars, at Teva USA.
With nearly 500 generic medicines available, Teva has the
largest portfolio of FDA-approved generic products on the market,
and holds the leading position in first-to-file opportunities, with
approximately 100 pending first-to-files in the U.S. Currently, 1
in 12 generic prescriptions dispensed in the U.S. is filled with a
Teva generic product.
Revlimid® had annual sales of $2.9 billion as of January, 2023,
according to IQVIA data.
What are lenalidomide capsules?
Lenalidomide capsules are a prescription medicine, used to treat
adults with:
- multiple myeloma (MM)
- in combination with the medicine dexamethasone
- a condition called myelodysplastic syndromes (MDS).
Lenalidomide capsules are for the type of MDS with a chromosome
problem where part of chromosome 5 is missing. This type of MDS is
known as deletion 5q MDS. People with this type of MDS may have low
red blood cell counts that require treatment with blood
transfusions.
- mantle cell lymphoma (MCL) when the disease comes back or
becomes worse after treatment with 2 prior medicines, one of which
included bortezomib. MCL is a cancer of a type of white blood cell
called lymphocytes that are in the lymph nodes.
Lenalidomide capsules should not be used to treat people who
have chronic lymphocytic leukemia (CLL) unless they are
participants in a controlled clinical trial.
It is not known if lenalidomide capsules are safe and effective
in children.
IMPORTANT SAFETY INFORMATION
What is the most important information I should know about
lenalidomide capsules?
Before you begin taking lenalidomide capsules, you must read and
agree to all of the instructions in the Lenalidomide REMS program.
Before prescribing lenalidomide capsules, your healthcare provider
will explain the Lenalidomide REMS program to you and have you sign
the Patient-Physician Agreement Form.
Lenalidomide capsules may cause serious side effects
including:
- Possible birth defects (deformed babies) or death of an
unborn baby. Females who are pregnant or who plan to become
pregnant must not take lenalidomide capsules.
Lenalidomide is similar to the medicine thalidomide. We
know thalidomide can cause severe life-threatening birth defects.
Lenalidomide capsules have not been tested in pregnant females.
Lenalidomide capsules have harmed unborn animals in animal
testing.
Females must not get pregnant:
- For at least 4 weeks before starting lenalidomide capsules
- While taking lenalidomide capsules
- During any breaks (interruptions) in your treatment with
lenalidomide capsules
- For at least 4 weeks after stopping lenalidomide capsules
Females who can become pregnant:
- Will have pregnancy tests weekly for 4 weeks, then every 4
weeks if your menstrual cycle is regular, or every 2 weeks if your
menstrual cycle is irregular.
- If you miss your period or have unusual bleeding, you will need
to have a pregnancy test and receive counseling.
- Must agree to use two acceptable forms of birth control at the
same time, for at least 4 weeks before, while taking, during any
breaks (interruptions) in your treatment, and for at least 4 weeks
after stopping lenalidomide capsules.
- Talk with your healthcare provider to find out about options
for acceptable forms of birth control that you may use to prevent
pregnancy before, during, and after treatment with lenalidomide
capsules.
- If you had unprotected sex or if you think your birth control
has failed, stop taking lenalidomide capsules immediately and call
your healthcare provider right away.
If you become pregnant while taking lenalidomide capsules,
stop taking it right away and call your healthcare provider. If
your healthcare provider is not available, you can call the REMS
Call Center at 1‐888‐423‐5436. Healthcare providers and patients
should report all cases of pregnancy to:
- FDA MedWatch at 1-800-FDA-1088, and
- The Lenalidomide REMS program at 1‐888‐423‐5436
There is a pregnancy exposure registry that monitors the
outcomes of females who take lenalidomide capsules during
pregnancy, or if their male partner takes lenalidomide capsules and
they are exposed during pregnancy. You can enroll in this registry
by calling the Lenalidomide REMS program at the phone number listed
above.
Lenalidomide can pass into human semen:
- Males, including those who have had a vasectomy, must always
use a latex or synthetic condom during any sexual contact with a
pregnant female or a female that can become pregnant while taking
lenalidomide capsules, during any breaks (interruptions) in your
treatment with lenalidomide capsules, and for up to 4 weeks after
stopping lenalidomide capsules.
- Do not have unprotected sexual contact with a female who is or
could become pregnant. Tell your healthcare provider if you do have
unprotected sexual contact with a female who is or could become
pregnant.
- Do not donate sperm while taking lenalidomide capsules, during
any breaks (interruptions) in your treatment, and for up to 4 weeks
after stopping lenalidomide capsules. If a female becomes pregnant
with your sperm, the baby may be exposed to lenalidomide and may be
born with birth defects.
Men, if your female partner becomes pregnant, you should call
your healthcare provider right away.
- Low white blood cells (neutropenia) and low platelets
(thrombocytopenia). Lenalidomide capsules cause low white blood
cells and low platelets in most people. You may need a blood
transfusion or certain medicines if your blood counts drop too low.
Your healthcare provider should check your blood counts often
especially during the first several months of treatment with
lenalidomide capsules, and then at least monthly. Tell your
healthcare provider if you develop any bleeding or bruising, during
treatment with lenalidomide capsules.
- Blood clots. Blood clots in the arteries, veins, and
lungs happen more often in people who take lenalidomide capsules.
This risk is even higher for people with multiple myeloma who take
the medicine dexamethasone with lenalidomide capsules. Heart
attacks and strokes also happen more often in people who take
lenalidomide capsules with dexamethasone. To reduce this increased
risk, most people who take lenalidomide capsules will also take a
blood thinner medicine. Before taking lenalidomide capsules, tell
your healthcare provider:
- If you have had a blood clot in the past
- If you have high blood pressure, smoke, or if you have been
told you have a high level of fat in your blood
(hyperlipidemia)
- About all the medicines you take. Certain other medicines can
also increase your risk for blood clots. Call your healthcare
provider or get medical help right away if you get any of the
following during treatment with lenalidomide capsules:
- Signs or symptoms of a blood clot in the lung, arm, or leg
may include: shortness of breath, chest pain, or arm or leg
swelling
- Signs or symptoms of a heart attack may include: chest
pain that may spread to the arms, neck, jaw, back, or stomach area
(abdomen), feeling sweaty, shortness of breath, feeling sick or
vomiting
- Signs or symptoms of stroke may include: sudden numbness
or weakness, especially on one side of the body, severe headache or
confusion, or problems with vision, speech, or balance
Who should not take lenalidomide capsules?
Do not take lenalidomide capsules if you:
- are pregnant, plan to become pregnant, or become pregnant
during treatment with lenalidomide capsules. See “What is the most
important information I should know about lenalidomide
capsules?”
- are allergic to lenalidomide or any of the ingredients in
lenalidomide capsules. See the end of the Medication Guide for a
complete list of ingredients in lenalidomide capsules.
What should I tell my healthcare provider before taking
lenalidomide capsules?
Before you take lenalidomide capsules, tell your healthcare
provider about all of your medical conditions, including if
you:
- have liver problems
- have kidney problems or receive kidney dialysis treatment
- have thyroid problems
- have had a serious skin rash with thalidomide treatment. You
should not take lenalidomide capsules.
- are lactose intolerant. Lenalidomide capsules contain
lactose.
- are breastfeeding. Do not breastfeed during treatment with
lenalidomide capsules. It is not known if lenalidomide passes into
your breast milk and can harm your baby.
Tell your healthcare provider about all the medicines you
take, including prescription and over-the-counter medicines,
vitamins, and herbal supplements. Lenalidomide capsules and other
medicines may affect each other, causing serious side effects. Talk
with your healthcare provider before taking any new medicines.
Know the medicines you take. Keep a list of them to show your
healthcare provider and pharmacist.
What should I avoid while taking lenalidomide
capsules?
- See “What is the most important information I should know about
lenalidomide capsules?”
- Females: Do not get pregnant and do not breastfeed while
taking lenalidomide capsules.
- Males: Do not donate sperm while taking lenalidomide
capsules, during any breaks (interruptions) in your treatment, and
for up to 4 weeks after stopping lenalidomide capsules.
- Do not share lenalidomide capsules with other people. It
may cause birth defects and other serious problems.
- Do not donate blood while you take lenalidomide
capsules, during any breaks (interruptions) in your treatment, and
for 4 weeks after stopping lenalidomide capsules. If someone who is
pregnant gets your donated blood, her baby may be exposed to
lenalidomide and may be born with birth defects.
What are the possible side effects of lenalidomide
capsules?
Lenalidomide capsules can cause serious side effects,
including:
- See “What is the most important information I should know about
lenalidomide capsules?”
- Increased risk of death in people who have chronic
lymphocytic leukemia (CLL). People with CLL who take
lenalidomide capsules have an increased risk of death compared with
people who take the medicine chlorambucil. Lenalidomide capsules
may cause you to have serious heart problems that can lead to
death, including atrial fibrillation, heart attack, or heart
failure. You should not take lenalidomide capsules if you have CLL
unless you are participating in a controlled clinical trial.
- Risk of new cancers (malignancies). An increase in new
(second) cancers has happened in patients who received lenalidomide
capsules and melphalan, or a blood stem cell transplant, including
certain blood cancers, such as acute myelogenous leukemia (AML),
and myelodysplastic syndrome (MDS) and certain other types of
cancers of the skin and other organs. Talk with your healthcare
provider about your risk of developing new cancers if you take
lenalidomide capsules. Your healthcare provider will check you for
new cancers during your treatment with lenalidomide capsules.
- Severe liver problems, including liver failure and
death. Your healthcare provider should do blood tests to check
your liver function during your treatment with lenalidomide
capsules. Tell your healthcare provider right away if you develop
any of the following symptoms of liver problems:
- yellowing of your skin or the white part of your eyes
(jaundice)
- dark or brown (tea-colored) urine
- pain on the upper right side of your stomach area
(abdomen)
- bleeding or bruising more easily than normal
- feeling very tired
- Severe skin reactions and severe allergic reactions can
happen with lenalidomide capsules and may cause death. Call your
healthcare provider right away if you develop any of the following
signs or symptoms during treatment with lenalidomide capsules:
- a red, itchy, skin rash
- peeling of your skin or blisters
- severe itching
- fever
- Get emergency medical help right away if you develop any of
the following signs or symptoms during treatment with lenalidomide
capsules:
- swelling of your lips, mouth, tongue, or throat
- trouble breathing or swallowing
- raised red areas on your skin (hives)
- a very fast heartbeat
- you feel dizzy or faint
- Tumor lysis syndrome (TLS). TLS is caused by the fast
breakdown of cancer cells. TLS can cause kidney failure and the
need for dialysis treatment, abnormal heart rhythm, seizure and
sometimes death. Your healthcare provider may do blood tests to
check you for TLS.
- Worsening of your tumor (tumor flare reaction) can
happen with lenalidomide capsules and may cause death. Tell your
healthcare provider if you get any of these symptoms of tumor flare
reaction during treatment with lenalidomide capsules: tender
swollen lymph nodes, low grade fever, pain, or rash.
Your healthcare provider may tell you to decrease your dose,
temporarily stop or permanently stop taking lenalidomide capsules
if you develop certain serious side effects during treatment with
lenalidomide capsules.
- Thyroid problems. Your healthcare provider may check
your thyroid function before you start taking lenalidomide capsules
and during treatment with lenalidomide capsules.
- Risk of Early Death in MCL. In people who have Mantle
Cell Lymphoma (MCL), there may be a risk of dying sooner (early
death) when taking lenalidomide capsules. Talk with your healthcare
provider about any concerns and possible risk factors.
The most common side effects of lenalidomide capsules
include:
- diarrhea
- rash
- nausea
- constipation
- tiredness or weakness
- fever
- itching
- swelling of your arms, hands, legs, feet and skin
- sleep problems (insomnia)
- headache
- muscle cramps or spasms
- shortness of breath
- cough, sore throat, and other symptoms of a cold
- upper respiratory tract infection or bronchitis
- inflammation of the stomach and intestine (“stomach flu”)
- nose bleed
- shaking or trembling (tremor)
- joint aches
- pain in your back or stomach-area (abdomen)
These are not all the possible side effects of lenalidomide
capsules. Call your doctor for medical advice about side effects.
You are encouraged to report side effects of prescription drugs to
the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
Please read the Medication Guide in the full Prescribing
Information including Boxed Warning.
About Teva
Teva Pharmaceutical Industries Ltd. (NYSE and TASE: TEVA) has
been developing and producing medicines to improve people’s lives
for more than a century. We are a global leader in generic and
innovative medicines with a portfolio consisting of over 3,500
products in nearly every therapeutic area. Around 200 million
people around the world take a Teva medicine every day, and are
served by one of the largest and most complex supply chains in the
pharmaceutical industry. Along with our established presence in
generics, we have significant innovative research and operations
supporting our growing portfolio of innovative and
biopharmaceutical products. Learn more at www.tevapharm.com.
Cautionary Note Regarding Forward-Looking Statements
This press release contains forward-looking statements within
the meaning of the Private Securities Litigation Reform Act of
1995, which are based on management’s current beliefs and
expectations and are subject to substantial risks and
uncertainties, both known and unknown, that could cause our future
results, performance or achievements to differ significantly from
that expressed or implied by such forward-looking statements. You
can identify these forward-looking statements by the use of words
such as “should,” “expect,” “anticipate,” “estimate,” “target,”
“may,” “project,” “guidance,” “intend,” “plan,” “believe” and other
words and terms of similar meaning and expression in connection
with any discussion of future operating or financial performance.
Important factors that could cause or contribute to such
differences include risks relating to the development and
commercial success of our generic version of Revlimid®
(lenalidomide capsules); our ability to successfully compete in the
marketplace, including, that we are substantially dependent on our
generic products, concentration of our customer base and commercial
alliances among our customers, delays in launches of new generic
products and the increase in the number of competitors targeting
generic opportunities and seeking U.S. market exclusivity for
generic versions of significant products; our substantial
indebtedness; our business and operations in general, including,
the impact of global economic conditions and other macroeconomic
developments and the governmental and societal responses thereto,
and costs and delays resulting from the extensive pharmaceutical
regulation to which we are subject; compliance, regulatory and
litigation matters, including failure to comply with complex legal
and regulatory environments; other financial and economic risks;
and other factors discussed in our Annual Report on Form 10-K for
the year ended December 31, 2022, including in the section
captioned “Risk Factors.” Forward-looking statements speak only as
of the date on which they are made, and we assume no obligation to
update or revise any forward-looking statements or other
information contained herein, whether as a result of new
information, future events or otherwise. You are cautioned not to
put undue reliance on these forward-looking statements.
1 Revlimid® is a registered trademark of Celgene Corporation, a
Bristol-Myers Squibb Company
View source
version on businesswire.com: https://www.businesswire.com/news/home/20230306005799/en/
IR Contacts
United States Ran Meir (267) 468-4475
Sanjeev Sharma (973) 658 2700
Israel Yael Ashman 972 (3) 914-8262
PR Contacts
United States Kelley Dougherty (973) 658-0237
Yonatan Beker (973) 264 7378
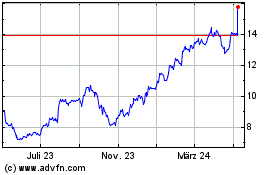
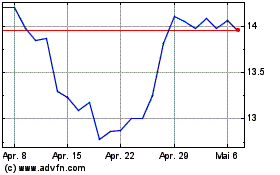
Teva Pharmaceutical Indu... (NYSE:TEVA)
Historical Stock Chart
Von Mär 2024 bis Apr 2024
Teva Pharmaceutical Indu... (NYSE:TEVA)
Historical Stock Chart
Von Apr 2023 bis Apr 2024